How to leverage peer-reviewed health science to build a physician referral base | Hearing Review July 2014
By Brian Taylor, AuD, and Bob Tysoe
“The people who think they are crazy enough to change the world are the ones who do so.”—Steve Jobs
In Part 1 of this series and in blog posts, we have touted the importance of obtaining “pillar of community” status and how it can be used to build a sustainable independent practice over the long term. This article will delve into a specific realm of pillar of community—your ability to form meaningful connections with primary care medicine. This approach is one component of interventional audiology, which we introduced in the November 2012 edition of Hearing Review.1
There are approximately 260,000 primary care physicians (PCPs) in the United States who influence 19% of the gross domestic product (GDP). This amounts to $2.7 trillion spent per year on healthcare in the United States.2 Each one of these primary care physicians has approximately 2,000 patients in his/her practice. Based on a review of National Institutes of Health (NIH) data, Lin et al3 estimated that 20.1% of Americans (48 million people) cannot pass a 25 dB hearing screening in either one or both ears using the World Health Organization’s standard hearing screening regimen.
Most hearing care professionals (HCPs) would agree that this degree of hearing loss is severe enough to interfere with daily communication. Although it may have taken awhile, other healthcare professionals—particularly physicians—are beginning to recognize the growing epidemic of age-related hearing loss and its impact on public health. The pertinent question is: Will the relatively small and obscure profession of audiology and hearing healthcare influence the practice of primary care medicine and nearly a fifth of a nation of more than 315 million people’s GDP?
The marvels of modern medicine are so ubiquitous that we often take them for granted. For example, average life expectancy of an American now approaches 79 years—an increase of more than 30 years since 1900!4 Individuals ages 70 to 75, those who are just now beginning to seek the services of audiologists on a massive scale, have scarcely experienced the premature death of siblings, friends, or neighbors, making this group unlike any other generation in history. Thanks to antibiotics, science-based clinical practices, and vaccinations, infectious diseases such as scarlet fever and influenza are no longer a possible death sentence for those afflicted with them. A consequence of this much longer lifespan is our ability as a society to manage the expenses of a rapidly aging population. The combination of a rapidly aging population, along with significant increases in the cost of medical care, has necessitated the changes we are beginning to see in how medical care is delivered in the United States.
These changes in the US healthcare system are huge opportunities for audiologists and dispensing professionals, especially in the context of the increasing awareness of age-related hearing loss as a public health concern. (See coverage of the Institute of Medicine’s January 2014 2-day workshop on “Age-related Hearing Loss and Healthy Aging” at: https://hearingreview.com/2014/02/iom-nrc-hosts-hearing-loss-and-healthy-aging-workshop.)
The growing awareness of age-related hearing loss as a public health concern represents a monumental opportunity for hearing care professionals to touch the lives of more patients in need of their services. This can only occur if we are willing to form partnerships with primary care physicians around the triple threat of untreated age-related hearing loss and the comorbid conditions associated with it. From a business perspective, a strategic alliance between audiologists and primary care physicians in communities across the country represents a sustainable revenue stream for clinicians willing to unbundle and charge for professional services. More importantly, from a patient’s perspective, early intervention of age-related hearing loss and its consequences has the potential to allow individuals the ability to maintain an active and participatory life as they age.
Let’s deconstruct this incredible opportunity to build bridges with the primary care physician community. Should a hearing healthcare provider establish a defined market of primary care doctors within a 5- to 10-mile radius from his/her practice (eg, 50 physicians), all of whom have 2,000 patients per practice, the target market is actually 100,000 patients—20.1% of whom have a potentially treatable loss. That amounts to 20,000 patients. Approximately 25% have already been treated for hearing loss,3,5 so 15,000 patients remain for hearing care professionals to find mutually beneficial ways to partner with primary care physicians in the comprehensive care of their patients.
The 4 Ps of Modern Healthcare: Preventive, Participatory, Preemptive, and Personalized
Due to changes in the American healthcare system, the practice of medicine is expected to see a marked increase in demand for services, especially for primary and preventive care. Because it is not possible to increase the supply of physicians in the short term (and in the long term, increasing the number of physicians is likely to increase the costs of delivering these types of services), the American healthcare system needs strategies for maintaining access in the face of increasing demand. In view of these proposed changes to the American healthcare system, physicians are now being encouraged to implement the following6:
1. Create primary care teams in which each member of the team functions at the highest level of her license.
2. Encourage self-care through better education of patients about their condition.
3. Organize seniors who can no longer live independently into patient-centered primary care homes in which the same physician or team of physicians orchestrates delivery of healthcare, so that the appropriate type of preventive services can be delivered in a consistent manner and duplication of services is minimized.
4. Use alternatives to a single patient-physician visit when possible, such as group visits for diabetic patients and the use of telemedicine.5,6
5. Eliminate unnecessary testing and overuse of medications.
These recommended changes in medical practice are a golden opportunity to demonstrate how audiology and hearing healthcare contribute to improving the overall quality of care of patients at risk for hearing loss, while reducing the overall costs to the entire healthcare system. This process starts with how audiologists and dispensing professionals fit into the larger picture of healthcare from the perspective of an entry point for hearing care, the primary care physician.
The transformation of healthcare to personalized, preventive, pre-emptive, and participatory is demanding audiologists, in particular, to rethink how they create value in the marketplace. In short, the future of audiology may be less dependent on dispensing a device and more dependent on our ability to offer personalized, preventive, pre-emptive, and participatory services to younger patients with milder hearing losses.
At the heart of this transformation from the device being the center of our universe to a myriad of diverse rehabilitative services taking center stage is our ability to effectively communicate with the medical community using the three traits shown in Figure 1.
Building Effective Relationships
In an era of smartphones and Skype, where global communication is instantaneous and almost free, there is something downright old-fashioned and quaint about how to build an effective relationship with the primary care physician community. After more than a decade of helping hearing care professionals build relationships with physicians, we believe the key drivers of an effective HCP-PCP relationship in which all parties, including patients, benefit are depicted in Figure 1. Let’s examine each of the three key drivers more carefully.
Authenticity. Ensuring to the PCP that you have the best interests of the patient as your highest priority begins with the ability to be authentic. Authenticity is best described as the ability to engender trust and respect in another person by putting your true self forward.
Due to our increasingly transparent world where information travels at lightning speed to anyone with an Internet connection who happens to be paying attention, the rhetoric of your marketing efforts must be congruent with the reality of how you interact with patients, the community, and other professionals, including PCPs. Other people quickly recognize when a marketing campaign centered around the promise of delivering a transcendent patient experience is overshadowed by the reality of an ordinary, high-pressure sales pitch revolving around hearing aids. In simple terms, authenticity means that you deliver on the promise of your marketing and advertising campaigns. Any disconnect between the two is likely to damage your reputation or brand. Being perceived as authentic—saying what you mean and meaning what you say—can only occur if you are visible within your community and credible in your communications.
Visibility. In a world in which your brand centers on the professional and not the devices you dispense, it is imperative you are visible to the entire community, especially PCPs. Despite all the efforts of hearing aid manufacturers, industry consultants, and buying groups to create glossy physician outreach materials, these materials still need to be delivered by the person who is going to be seeing the patient.7 Taking no more than 2 hours per week to personally visit a PCP practice is a proven approach to becoming more visible and building your brand image.
Credibility. The final section of the PCP relationship triangle is credibility. In short, a credible professional is one who knows the latest science as it relates to hearing loss and amplification and can apply it to clinical practice. From the perspective of building relationships with the PCP community, credibility relates to the fact that you can read, evaluate, apply, and articulate the peer-reviewed research pertaining to age-related hearing loss and its myriad comorbidities. Physicians are trained in the scientific method and are taught in medical school to evaluate new information with healthy skepticism. Therefore, any communication or attempt to educate medical professions must be grounded in well-reasoned evidence.
Arm Yourself with Data: Five Studies You Need to Understand
Hearing care professionals would be wise to read these five studies, which use well-designed methods and have been published in peer-reviewed journals within the past 2 years, and cite their relevant findings in any professional communication with PCPs.
1) Lin F, et al. Hearing loss and cognitive decline in older adults. JAMA Internal Medicine. 2013;173(4):293-299. A total of 1,984 adults between the ages of 70 and 79 were followed up to 12 years in order to evaluate whether hearing loss is independently associated with accelerated cognitive decline. Cognitive testing consisted of the Digit Symbol Substitution (DSS) test and the 3MS, which are two standardized tests of cognitive function in adults.
Results indicated that 1,162 individuals with baseline hearing loss had a 32% poorer score on the DSS and a 41% poorer score on the 3MS compared to those with normal hearing. Compared to those with normal hearing, individuals with hearing loss at baseline had a 24% increased risk for incident cognitive impairment.
The authors concluded that hearing loss is independently associated with accelerated cognitive decline and incident cognitive impairment in older adults. On average, individuals with hearing loss would require 7.7 years to decline by 5 points of the 3MS, while individuals with normal hearing experienced a 5 point decline over a 10.9 year period. Furthermore, the authors indicated that a 25 dB hearing loss equates to 7 years of cognitive decline when compared to a similar age group with normal hearing.
2) Fisher D, et al. Impairments in hearing and vision impact on mortality in older people. Age and Aging. 2014;43(1):69-76. The main objective of this study was to examine the relationship between hearing and vision impairments and mortality from all-cause (all-cause mortality by age group is the annual number of deaths in a given age group per the population in that age group, usually expressed per 100,000) and cardiovascular disease among older people. All 4,926 study participants were from Iceland and 67 years of age or older.
Participants were placed into one of three categories: vision-only impairment (VI), hearing-only impairment (HI), and dual sensory impaired (DSI), and they were followed up to 7 years. After adjusting for age, significantly increased mortality from all-cause and cardiovascular disease was observed for the HI and DSI, especially among men. After further adjustment for mortality risk factors, individuals with HI remained at higher risk for death from cardiovascular disease.
Whether hearing loss is an indicator of aging or frailty, physical manifestations resulting in reduced social competence, or a reflection of other adverse health status is unclear. However, results indicated that older men with DSI or HI were at a significantly greater risk for all-cause and cardiovascular death. Regular hearing assessments and rehabilitation services at an earlier age in order to promote long-term health and longevity are warranted based on these findings.
3) Mick P, et al. The association between hearing loss and social isolation in older adults. Otolaryngology-Head & Neck Surgery. 2014;150:378-384. The objective of this study was to determine if age-related hearing loss is associated with social isolation, and whether factors such as age, gender, and hearing aid use moderate this association. There were 1,453 male and female participants in this study, all between the ages of 60 and 84 years. Social isolation was defined using the social isolation score (SIS).
Results indicated that greater amounts of hearing loss were associated with increased odds of social isolation in women aged 60 to 69. Other groups did not show a significant relationship between hearing loss and social isolation. These results suggest that women within this age range are more likely to alter their lifestyle due to their hearing loss; thus, they are more likely to become socially isolated.
4) Chuan-Ming L, et al. Hearing impairment associated with depression in US adults, NHANES 2005-2010. Otolaryngology-Head & Neck Surgery. 2014;140(4):293-302. This study estimated the prevalence of depression among adults with hearing loss. Using the 9-item Patient Health Questionnaire (PHQ-9), the prevalence of depression among 18,318 participants of the National Health and Nutrition Examination Survey (NHANES) was examined.
The prevalence of depression increased as hearing loss became worse, except among those self-reported as deaf. Among individuals over the age of 70, no significant association between self-reported hearing loss and depression was found. Adults under the age of 70, particularly women, had a significant association between moderate hearing loss and depression.
5) Lin F, et al. Association of hearing impairment with brain volume changes in older adults. Neuroimage. 2014;90:84-92. Brain volume changes were monitored for a mean span of 6.4 years in 126 adults between the ages of 56 and 86. Using sophisticated brain volume measurement techniques, and after adjusting for cardiovascular and demographic factors, the researchers found that individuals with hearing loss had accelerated brain volume declines. These declines in brain volume were primarily confined to the right temporal lobe.
The findings of this study indicate that peripheral hearing loss is independently associated with accelerated brain atrophy in whole brain and regional volumes concentrated in the right temporal lobe.
Taken as a whole, these five studies suggest that age-related hearing loss has implications well beyond affecting basic communication skills. Although remediating these basic communication skills through early identification using hearing screening has merit in its own right, these five studies provide a high level of evidence demonstrating broader functional implications of age-related hearing impairment on cognitive function, depression, social isolation, cortical changes in the brain, and even early death.
Hearing care professionals have a professional obligation—perhaps bordering on a moral imperative—to communicate these findings without hyperbole, inaccuracy, or embellishment. Each study cited here stands on its own as an outstanding contribution to our evolving understanding of the relationship between age-related hearing loss and other common chronic conditions associated with the aging process. By understanding the design of each study, appreciating each study’s limitations, and not exaggerating the authors’ conclusions, we can begin to develop an evidence-based core message, likely to resonant with the primary care medical community.
Audiologists and hearing care professionals would be wise to develop this core message independent of marketers, who may be tempted to embellish the message, thus jeopardizing our credibility.
The Core Message After reading these five recently published papers and evaluating their findings using your ability to deconstruct each study’s design and conclusions, it is likely that you will be able to craft a succinct message similar to the one below. After tailoring it to your liking, the next step is to infuse this message in all your personal communication with the PCP community.
“Age-related hearing loss (AHL) is a public health concern of very high priority. It’s a high priority because several recent studies using randomized-controls show AHL contributes to the acceleration of cognitive and physical decline in adults. Hearing loss imposes a heavy social and economic burden on individuals, families, and communities, as a hearing loss isolates people. Given these findings, all individuals over the age of 50 should have a baseline hearing screening, and patients with a history of depression, cardiovascular disease, diabetes, and dementia should have their hearing screened annually.”
Implementation: Systematically Communicating with PCPs The next questions for hearing care professionals who want to form a strong strategic relationship with primary care medicine are: 1) How can I help these patients get the care they so obviously need? and 2) Is my unique market underserved, and will I be rewarded for investing my time and resources in trying to add new patients to my practice with “physician marketing” strategies? The answer to these questions largely resides in your ability to implement a pillar of community communication strategy in place for your practice.
Historically, marketing research? and testimonials from audiologists who have implemented a physician outreach program support the conclusion that the risk is worth taking, and that you will be adequately rewarded.
Pharmaceutical industry marketing research shows it takes five to six calls on a physician to generate a prescription for a new drug. It takes the same number of calls to a primary care physician to generate a new patient referral for an audiologic evaluation. Based on our experience, the number of calls required decreases over time as the relationship between the HCP and PCP evolves.
Currently, the average US audiology clinic generates $400,000 per year in annual revenue, of which 15% ($60,000) is derived from patients who have been referred by a physician. If one could double the percentage of physician referrals—a very attainable goal based on our experience—then total revenue from physicians becomes $120,000, of which $60,000 is new income.
To equal this return on investment (ROI), you would need to have $1,000,000 invested in the stock market with an annual return of 12%. For those of you who are not high-risk investors, this may not even be attainable, assuming of course that you have a discretionary $1 million to give to your stockbroker.
Let’s revisit the 12,750 patients who will test with hearing loss (TWHL), and assume that all are referred to a hearing healthcare specialist. We will project that the average number of TWHL referrals to obtain a binaural hearing aid fitting is three, then there are 4,250 patients who will purchase a pair of instruments. At an average of $5,000 per set, the total dollar value of the attainable target market is $2,125,000.
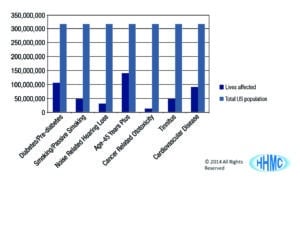
Again, we must ask the question, “Which are those patient types that are in a high-risk patient category over the age of 12 years who should be tested?” The answer lies with those patients with the presence of coexisting conditions or comorbidities that contribute to the cause of, and increased incidence of, hearing loss. By the numbers they are:
- 106,000,000 people in the United States who are either diabetic (twice the incidence) or prediabetic (30% increase in the incidence) who have up to 2 times the incidence of hearing loss versus those who do not have diabetes or prediabetes.5 (Although we did not cite any recent studies showing the relationship between Type II diabetes and hearing loss, there are several, including Bainbridge5 and Parker.8)
- 48,000,000 Americans smoke cigarettes. Smokers have 2 times the incidence of hearing loss versus nonsmokers, and secondhand smokers have a 1.7 time incidence of hearing loss versus non-secondhand smokers.9
- 30,000,000 of the US working population are exposed to on-the-job toxic noise levels above the OSHA standard of 85 dB every day.10
- 140,000,000 Americans are older than age 45, with 10,000 turning 65 every day.11 Over 30% of the age 65+ group have a treatable loss, and this number increases with advancing age.
- 12,000,000 people in the United States currently have cancer, and over 50% will be treated with chemotherapy, which may include cisplatin-based derivative drugs. Almost 100% will suffer high frequency hearing loss post cessation of chemotherapy.12
- 50,000,000 to 60,000,000 Americans suffer from tinnitus, and approximately 90% have concomitant hearing loss.13
- 80,000,000 suffer from cardiovascular disease and the disease’s many complications that include 3 times the incidence of hearing loss (versus the patient who does not have cardiovascular disease). Hypertension, a subcategory of cardiovascular disease that is now the most prevalent treatable chronic disease in the United States and the world, is a proven cause of hearing loss.14 Figure 2 shows the prevalence of these various medical conditions in relation to the total population of the United States.
Pillar of Community Marketing
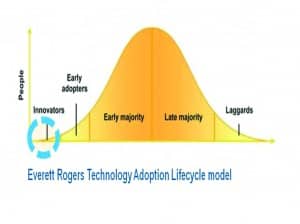
A pillar of community marketing strategy comprised of a physician outreach component is a long-term marketing strategy requiring commitment for the entire life of the practice (Figure 4). Given the second author’s previous experience working for a leading pharmaceutical company, let’s take a look at how those lessons may or may not apply to physician outreach for the HCP.
In the United States, the pharmaceutical industry’s experience when marketing new medications to physicians so that they will write prescriptions for the new drugs closely follows the bell curve in Figure 3.2 Physician outreach programs initiated by the hearing care industry in the United States, and validated by BHI MarkeTrak data and Hearing Healthcare Marketing Company, verify the identical experience in generating new patient referrals.7
Approximately 5% of physicians are “Innovators” and “Early Adopters.” In the first 6 months, this group will listen and readily initiate new patient care strategies because of your messaging regarding which patient types need audiologic care.
However, there are not enough of these physician types in your target market to make a ROI feasible for the long term.
The real rewards are in the “Early Majority” and “Late Majority” category of customers. It will take approximately 3 years to get to the top of the bell curve with a consistently implemented physician marketing program. You will have another 3 to 5 years of peak sustainable revenue, and increasingly profitable returns on your time and resources invested.
If there is a single message gleaned from Figure 3, it is that you must make a commitment to educate the early and late majority of adoptors. This can take 2 to 3 years based on our experience, but by using the findings from well-designed clinical studies showing the comorbid relationship between hearing loss and other common chronic conditions, you have quality material to sustain those efforts.
New hearing care technological innovations, enlightened joint clinical research by physicians and audiologists, and expanded services that differentiate you and your practice’s patient care capabilities will allow you to maintain a “top of the mind” presence in physicians’ clinics, generating another revenue stream and potentially bringing in younger patients for preemptive care.
Now is the time to boldly instill these ideas into your practice by initiating calls and developing relationships with the receptionists, referral coordinators, medical assistants and nurses, primary care physicians, and their office managers. Tailor the core message mentioned above in an authentic manner in order to build credibility and trust. Ask PCPs to heed our patient care calls to action, and accept us as part of the patient care team that seeks to minimize impairment and maximize function in adults with age-related hearing loss.
The peer-reviewed articles cited here provide a rational argument. Are you bold enough to bring it to life within your practice and crazy enough to change the world?
Correspondence can be addressed to Dr Taylor at: [email protected]
References
1. Taylor B, Tysoe B. Interventional audiology: partnering with physicians to deliver integrative and preventive hearing care. Hearing Review. 2013;20(12)[Nov]:16-22.
2. Tysoe R. Disease state marketing. Audiology Practices. 2012;4(1):22-28.
3. Lin F. Hearing loss prevalence in the United States. Arch Intern Med. 2011;171(20):1851-1852. Available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3564588
4. Countryeconomic.com. United States—Life expectancy at birth. Available at: www.countryeconomy.com/demography/life-expectancy/usa
5. Bainbridge K. Diabetes and hearing impairment in the United States: audiometric evidence from the National Health and Nutrition Examination Surveys, 1999–2004. Ann Intern Med. 2008;149(1):1-10.
6. Katz M. Health insurance is not health care. JAMA Internal Med. 2014;April 7, e1-e2. Available at: http://archinte.jamanetwork.com/article.aspx?articleid=1857087
7. Kochkin S. BHI physician program found to increase use of hearing healthcare. Hear Jour. 2004;57(8):27-29.
8. Parker P. Diabetes and hearing loss. Audiology Practices. 2009;2(4):22-23.
9. Katbamna B. Effects of smoking on the auditory system. Audiology Online, October 28, 2008. Available at: http://www.audiologyonline.com/articles/effects-smoking-on-auditory-system-899
10. May JJ. Occupational hearing loss. Am J Ind Med. 2000;37:112-120.
11. 2013 United States Census Bureau. Available at: http://www.census.gov
12. American Cancer Society. Cisplatin. Available at: http://www.cancer.org/treatment/treatmentsandsideeffects/guidetocancerdrugs/cisplatin
13. Fausti SA, Wilmington DJ, Helt PV, Helt WJ, Konrad-Martin D. Hearing health and care: the need for improved hearing loss prevention and hearing conservation practices. J Rehab Research Development. 2005;42(4):45-62. Available at: www.rehab.research.va.gov/jour/05/42/4suppl2/pdf/fausti.pdf
14. de Moraes Marchiori LL, de Almeida Rego Filho E, Matsuo T. Hypertension as a factor associated with hearing loss. Braz J Otolaryngol. 2006;72:533-40.
Original citation for this article: Taylor B, Tysoe B. Forming strategic alliances with primary care medicine: interventional audiology in practice: How to leverage peer-reviewed health science to build a physician referral base. Hearing Review. 2014;21(7):22-27.