In two new studies, USC Stem Cell scientists explain why sensory hearing cells of the inner ear don’t regenerate after damage and how we might be able to change it. The studies were partially funded by the National Institutes of Health and published in the Proceedings of the National Academy of the Sciences (PNAS).
“In the non-sensory supporting cells of the inner ear, key genes required for conversion to sensory cells are shut off through a process known as ‘epigenetic silencing.’ By studying how the genes are shut off, we begin to understand how we might turn them back on to regenerate hearing,” says John Duc Nguyen, the first author of one of the papers. Nguyen now works at the biotech company Genentech and earned his PhD in the USC Stem Cell laboratory of Neil Segil, who passed away from pancreatic cancer in 2022.
The second paper explored when and how the ability to form sensory hearing cells is gained in the inner ear in the first place and describes two specific genes that could be useful for regenerating hearing in adults.
“We focused on the genes Sox4 and Sox11 because we found that they are necessary for forming sensory hearing cells during development,” says the paper’s first author Emily Xizi Wang, who also conducted her research as a PhD student in the Segil Lab and works at the biotech company Atara Biotherapeutics.
“These two papers are not only great science, but also a clear example of Neil Segil’s enduring legacy as an exceptional mentor to the next generation of stem cell researchers,” says Gage Crump, a co-author on both papers and the interim chair of USC’s Department of Stem Cell Biology and Regenerative Medicine at the Keck School of Medicine of USC.
Study Focus: Gene Silencing
One important way that genes are shut off or “silenced” involves chemical compounds called methyl groups that bind to DNA and make it inaccessible—the focus of Nguyen’s paper. When the DNA that instructs a cell to become a sensory hearing cell is methylated, the cell cannot access these instructions.
Through their experiments with non-sensory supporting cells extracted from the inner ears of mice, Nguyen and his colleagues confirmed that DNA methylation silences genes that promote conversion into sensory hearing cells, including the gene Atoh1 that is known to be a master regulator of inner ear development.
An enzyme called TET can remove methyl groups from the DNA, thus reversing the gene silencing and restoring the capacity of supporting cells to convert into sensory hair cells. Accordingly, when the scientists blocked the activity of TET, the supporting cells retained their DNA methylation and therefore could not convert into sensory hair cells in the Petri dish.
Intriguingly, in a separate experiment, the researchers tested the extent of gene silencing in supporting cells from a chronically deafened mouse. They found that gene silencing was partially reversed, meaning that the supporting cells had the capacity to respond to signals to transform into sensory hearing cells. This finding has important implications: the loss of sensory hearing cells itself might partially reverse gene silencing in supporting cells in chronically deaf individuals. If so, the supporting cells of chronically deaf individuals might already be naturally primed to convert into sensory hearing cells.
Segil’s longtime collaborator Andrew K. Groves from the Baylor College of Medicine served as the paper’s corresponding author.
Analyzing Sox4 & Sox11
In the second paper, Wang and her colleagues explored when and how the progenitor cells of the inner ear gain the ability to form sensory hearing cells.
The scientists pinpointed when progenitor cells acquire this ability: between days 12 and 13.5 of embryonic development in mice. During this window, the progenitor cells acquire the capacity to respond to signals from the master regulator gene Atoh1 that triggers the formation of sensory hearing cells later during development.
What primes the progenitor cells to respond to Atoh1 are two additional genes, Sox4 and Sox11, that change the state of these cells.
In embryonic mice lacking Sox4 and Sox11, progenitor cells in the inner ear failed to develop into sensory hearing cells. Specifically, a loss of Sox4 and Sox11 made the cells’ DNA inaccessible—an effect similar to DNA methylation. With their DNA inaccessible, the progenitor cells couldn’t respond to signals from Atoh1.
On the flip side, high levels of Sox4 and Sox11 activity stimulated mouse progenitor cells and supporting cells to form sensory hearing cells in a Petri dish.
Further reading: Researchers Reverse Hearing Loss in Mice
More promising still, in mice with damaged sensory cells in the inner ear, high levels of Sox4 and Sox11 activity increased the percentage of vestibular supporting cells that converted into sensory receptor cells—from 6% to 40%.
“We’re excited to continue exploring the mechanisms by which cells in the inner ear gain the ability to differentiate as sensory cells during development and how these can be used to promote the recovery of sensory hearing cells in the mature inner ear,” says the paper’s corresponding author Ksenia Gnedeva, who completed her postdoctoral training in the Segil Lab and is now an assistant professor in the USC Tina and Rick Caruso Department of Otolaryngology – Head and Neck Surgery, and the Department of Stem Cell Biology and Regenerative Medicine.
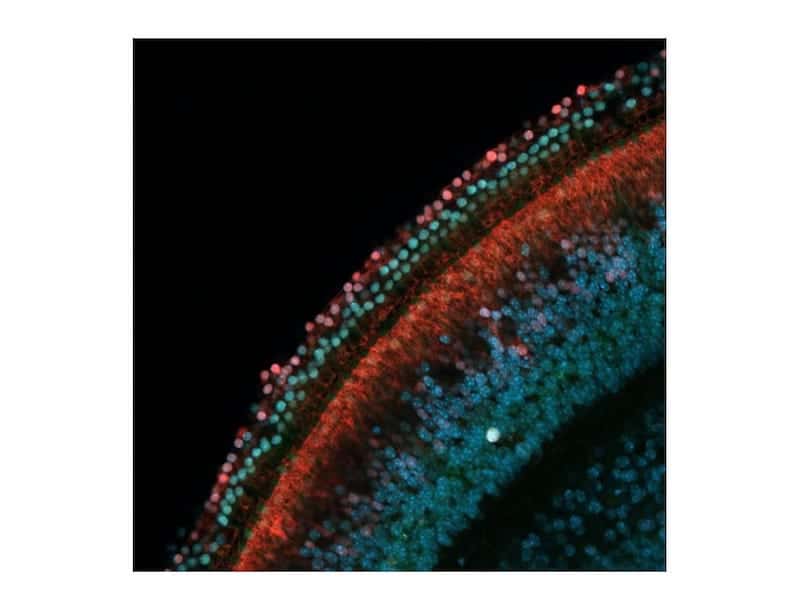
Featured image: Rows of sensory hearing cells (green) next to supporting cells (red) in the inner ear of a mouse. Photo: John Duc Nguyen and Juan Llamas/Segil Lab