By Cammy Bahner, MS; Michelle Petrak, PhD; Douglas L. Beck, AuD; and Amanda Smith, AuD
Part 3 of this 3-part series explores the relative contributions and importance of bi-thermal caloric testing as well as the contribution of whole body rotation.
This article is the third and final installment of the series titled “In The Trenches,” which has explored and elaborated on the clinical usefulness and applicability of various tools and protocols for the evaluation and management of the vestibular patient. In Part 3, we explore the relative contributions and importance of bi-thermal caloric testing, as well as the contribution of whole body rotation.
1) Caloric Tests
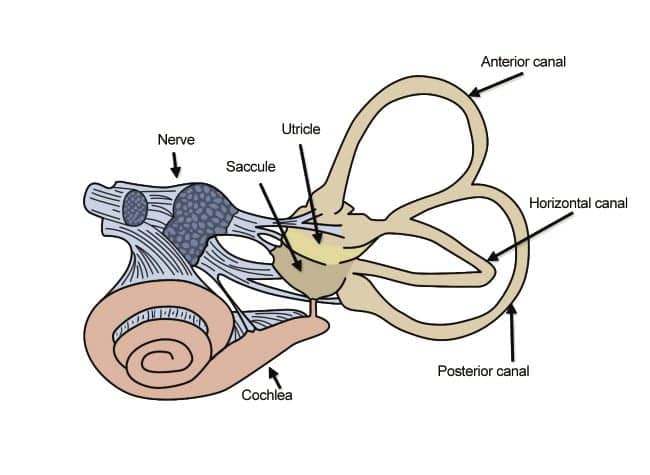
Bi-Thermal Caloric Irrigation is the “gold standard” test of vestibular end-organ function. The bi-thermal caloric test protocol essentially consists of four water-or-air “irrigations” of the external auditory canals. The core concept of bi-thermal irrigation is that when the stimulus (water or air) is significantly above/below body temperature, the temperature gradient initiates a “caloric” response via the horizontal canal (Figures 1 and 2). For water-based irrigations, the temperature of the water is ±7 degrees above/below body temperature. For air-based irrigations, the temperature gradient is increased. However, there is currently no ANSI standard temperature for air irrigations (see manufacturer’s specifications).
|
| Figure 1. Bi-thermal irrigation relies on temperature gradients caused by water or air in the external auditory canals, initiating a caloric response via the horizontal canal. |

|
| Figure 2. Air Fx Air Irrigator |
The central vestibular system relies on the peripheral vestibular system to provide adequate and equal input from each end organ. Caloric irrigation is used to assess the symmetry of the peripheral vestibular system and to document the excitatory/inhibitory response of each vestibular end organ.
When an asymmetry of the peripheral end organs exists, or when there is insufficient information from the peripheral end organs, the central nervous system compensates—resulting in nystagmus (eye motion).
Bi-thermal caloric irrigation is used to stimulate each vestibular end organ (independently) to determine whether one is weaker (or performing more poorly) than the other (asymmetry), and to verify each end organ is providing sufficient vestibular information to the brain. When neither vestibular end organ is functioning normally, the result may be a bilateral weakness.
The bi-thermal caloric analysis is based on measuring the nystagmus that occurs in response to thermal changes within the ear canal. Schmiederkam1 first described nystagmus secondary to ear canal irrigation. Robert Bárány2 won a Nobel Prize for his research in caloric stimulation. He proposed that, when a temperature gradient is generated across the horizontal semicircular canal (by irrigating the external auditory canal with a stimulus warmer or cooler than body temperature), the relative density of the endolymph changes. Thus, an ampullopetal (toward the ampulla) deflection of the cupula is generated with warm irrigations because the endolymph becomes lighter and rises, causing an excitatory response. Likewise, an ampullofugal (away from the ampulla) deflection is generated with cool irrigations, causing an inhibitory response with decreased afferent discharge.3
The nystagmus resulting from caloric irrigation can be measured by traditional electronystagmography (ENG) or videonystagmography (VNG) as described by Smith, Beck, Petrak, and Bahner4 in the November 2012 HR. For each of the four caloric subtests, the eye movements are recorded and the direction of the slow phase velocity (SPV) of the nystagmus is recorded.
The acronym “COWS” (Cold Opposite, Warm Same) helps recall the expected, normal results. Specifically, a cold stimulus in the left ear produces right beating (ie, opposite) nystagmus, and a warm stimulus in the left ear produces a left-beating (ie, same) nystagmus. A fully functional peripheral vestibular end organ will respond to stimulation approximately 15-30 seconds post-irrigation onset. The peak/maximum (averaged) response generally occurs 60-90 seconds post-irrigation onset and is recorded and used in the calculations that follow.
Total Caloric Response. The total caloric response is calculated based on the sum of the peak SPVs of all four irrigations; left warm (LW), left cold (LC), right warm (RW), and right cold (RC). Although there are differences of opinion as to what the minimal and maximal total caloric response should be, it is well accepted that a bilateral weakness is present if the total caloric response is less than 25 degrees per second, or if the total left (or right) ear response is less than 12 degrees per second.3 Likewise, hyperactive responses are considered to be present when SPVs from the total left (or right) ear response are greater than 140 degrees per second.5
Unilateral Weakness. A unilateral weakness (UW), also referred to as percent reduced vestibular response (%RVR, see ANSI/ASA S3.45-2009),6 is the ratio of the sum of the peak SPV of the right ear warm and right ear cool responses, minus the sum of the peak SPV of the left ear warm and left ear cool responses, divided by the total of all four peak SPV responses, or:
| UW = | (RW+RC) – (LW+LC) |
| RW+RC+LW+LC |
…then multiply result by 100 to convert to percentage.
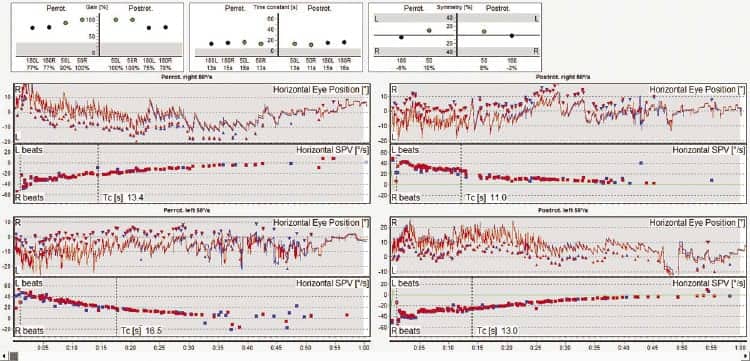
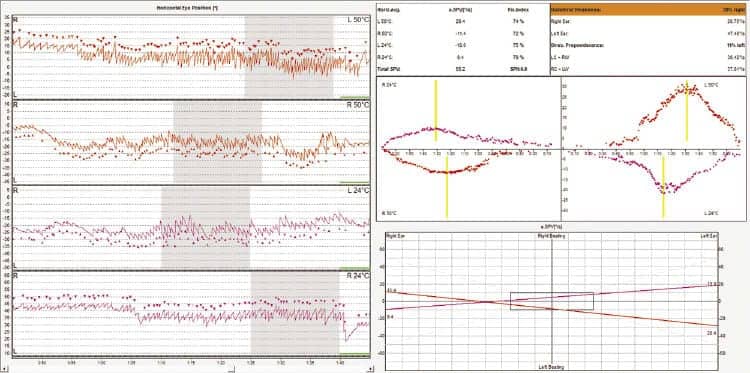
A difference between ears of 25% is the common value used clinically as the normal limit for UW (Figure 3).3 A difference greater than or equal to 25% is indicative of a clinically significant unilateral weakness in the ear producing the lesser responses (Figure 4).

|
| Figure 3. Example of “normal” caloric test results. (Click to enlarge) |
|
| Figure 4. Example of left unilateral weakness. (Click to enlarge) |
Directional Preponderance (DP).Directional preponderance is a measure of the “direction” fixed responses (ie, a comparison of the quantity of right-beating nystagmus compared to the quantity of left-beating nystagmus). The RW and LC responses both produce right-beating fast phases and the LW and RC produce left-beating fast phases. DP is the ratio of the sum of the peak SPV for the right-beating responses, minus the sum of the peak SPV for left-beating responses, divided by the total of all four peak SPV responses. When a positive value is obtained, it indicates that right-beating responses were stronger than left-beating responses.
| DP = | (RW+LC) – (LW+RC) |
| RW+LC+LW+RC |
…then multiply result by 100 to convert to percentage.
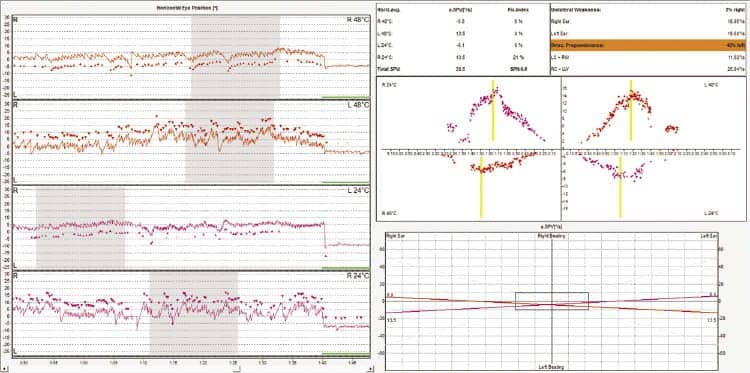
A directional preponderance value of 30% or greater is generally used to suggest the presence of a DP (Figure 5). DP is most often seen in acute impairments in which spontaneous nystagmus is present secondary to an uncompensated unilateral vestibular deficit.
|
| Figure 5. Example of directional preponderance to the left. (Click to enlarge) |
Spontaneous nystagmus skews the results of the caloric test and must be accounted for by adding (or subtracting) the numeric value of the spontaneous nystagmus from each caloric subtest (note that some software systems automatically correct for spontaneous nystagmus). Spontaneous nystagmus is almost always “direction-fixed” and will therefore “add” to responses in the direction of the spontaneous nystagmus fast phase and “reduce” the responses in the direction opposite the fast phase.
For example, a 5 degree right-beating spontaneous nystagmus will add “5” to the value of both the RW and the LC responses. Therefore, to correct for this, “5” should be subtracted from each of those peak SPV values so as to not report a DP, which was actually due to spontaneous nystagmus. Likewise, for the RC and LW responses, the effect would be the opposite (ie, “5” would be added to each subtest to correct for spontaneous nystagmus.
Fixation Suppression. Another formula of interest with respect to caloric irrigation is the fixation suppression index (FI). The FI is a ratio of the nystagmus intensity before and nystagmus intensity after the patient fixates on a target.7 The FI is calculated for at least one right-beating (rb) test and one left-beating (lb) test, and is expressed by:
| %FIrb = | Fix RW or LC | x 100 |
| NoFix RW or LC |
| %FIlb = | Fix LW or RC | x 100 |
| NoFix LW or RC |
McCaslin7 reports it is important that fixation suppression be administered immediately after the peak caloric response is reached, requiring constant monitoring of the response by the audiologist. If the patient is able to fully suppress nystagmus from the caloric response once a fixation target is introduced, the FI will be 0%. A FI of 100% would indicate no fixation. A failure to suppress nystagmus with fixation is a sign of a central vestibular pathology. Although there is no published normative value for FI, a common “normal” response limit seems to be about 60% (Table 1).

|
| Table 1. Common normative values for caloric response parameters. Adapted from Jacobson & Shepard 2008.5 (Click to enlarge table) |
Physical Examination of Ear Canal. A thorough examination of the external ear canal is necessary prior to caloric irrigation. Two important factors to consider are the presence of anatomical abnormalities (eg, tympanic membrane perforation, unusually shaped/tortuous ear canal, pressure equalization [PE] tubes) and the presence of cerumen. If excessive cerumen is present, it will preclude the stimulus from generating a sufficient temperature gradient across the horizontal canal of the irrigated ear and may prohibit a reliable test result.7 Without a thorough examination of the ear canal, it is impossible to know whether the achieved test results are an accurate assessment of the vestibular system.
Patient Positioning. It is necessary to perform VNG caloric irrigation with the patient in a vision-denied state to disallow fixation suppression of the nystagmus response. The patient needs to be positioned such that the head is at a 30° angle in order to bring the horizontal semicircular canals into a vertical position and aligned with the plane of gravity.
Alerting Tasks. Alerting tasks are necessary to discourage the patient from suppressing the nystagmus response. The most effective alerting tasks require the patient to use recall memory. For example, the audiologist might ask, “Name a state that begins with the letter ___”, “name a color that begins with ___”, “name a city in the state of ____”, etc.
Irrigation Order. The order in which the irrigations are performed is thought to be (essentially) clinically irrelevant. However, the consensus is that it is best to start with warm irrigations, which provide an excitatory response.
Some patients cannot tolerate bi-thermal irrigation. Therefore, if one starts with warm irrigations, at least a Monothermal Warm Screening Test (MWST) can be performed. (Note: The MWST should only be used if no other abnormalities are identified in the vestibular evaluation.7) MWST represents a percentage of asymmetry derived from only the warm-caloric irrigation responses. MWST also offers good sensitivity and specificity with respect to approximating the bi-thermal caloric test (83% and 90%) in children ages 6-14 years.
MWST is calculated as follows:
| MWST = | RW – LW |
| RW + LW |
…then multiply result by 100 (to convert to a percentage).
Because the VNG procedure requires detailed instruction and is sometimes distressing to the patient, it can be challenging to perform on children. However, the caloric test can be modified to create a more comfortable experience for the child.9 Further, for children under age 6 years, rotational chair testing may offer a better solution.
2) Rotational Chair Tests
Rotational chair tests evaluate the entire vestibulo-ocular reflex (VOR). Unlike caloric testing in which each ear is independently evaluated, tests involving rotational chairs test both ears simultaneously. Rotational chair testing (RCT) is much more sensitive than caloric testing for identifying vestibular deficits (71% sensitivity for RCT, compared to 31% for calorics).10 However, because the ears are not stimulated independently, RCT specificity is only 54%, compared to 86% specificity for calorics.10 When paired with bi-thermal caloric irrigations, rotary chair testing can provide the examiner additional information about the status of the patient’s vestibular system—leading to a more accurate diagnosis and, therefore, more effective treatment.
Bárány was the first to describe observable post-rotary nystagmus following rotation in a manually operated rotational chair in the early 1900s. He measured the duration of post-rotary nystagmus following 10 chair rotations over a 20-second period, and he observed differences in the nystagmus for clockwise versus counterclockwise rotations. Bárány reported difficulty with controlling the manual stimulus, as well as various effects from visual suppression (for details, see Jacobson and Shepard 2008, pages 253-254).5
In 2013, whole body rotation is performed with sophisticated computerized rotational chairs to control many of the variables introduced by manual stimulation. The patient is seated in a motor-driven rotational chair with the head bent slightly forward (30°) and secured with a head restraint to maintain the horizontal semicircular canals on the selected plane of rotation. The patient is tested with eyes open in total darkness while performing mental alerting tasks. Infrared goggles are placed on the patient’s eyes to monitor and record eye movements during rotational chair tests. In each subtest, nystagmus is recorded by the infrared camera (within the goggles) and a permanent graphical tracing of the nystagmus is obtained.
Previously, RCT was conducted within a dark room/booth (ie, fixation-free) to eliminate visual suppression of the nystagmus. With advances in modern VOG goggles that eliminate fixation, it is now possible to perform RCT in an open and lighted environment. Any light source visible to the patient can facilitate fixation and greatly reduce the VOR responses obtained.7 With the advent of open chair designs that recline to various positions for positional and caloric testing, one can perform the entire VNG examination from the rotary chair (Figures 6a-b).

|

|
| Figure 6a-b. There are several clinical applications for RCT. RCT is particularly useful for difficult-to-test populations, such as testing pediatric patients to determine the severity of bilateral weakness. Cyr (1980) successfully performed RCT on infants as young as 3 months of age. RCT also can be performed on patients with middle ear pathology, unlike bi-thermal caloric stimulation, which is generally not possible for those patients. Specifically, patients with TM perforations, middle ear effusion, or a history of mastoidectomy can be evaluated via RCT. | |
A very important advantage of RCT is its usefulness in determining whether a unilateral weakness is compensated or uncompensated. When evaluating the vestibular system with caloric testing only, it is more difficult to determine whether compensation has occurred because a unilateral weakness will always be present with caloric stimulation. However, a patient with a compensated unilateral weakness will present with normal Sinusoidal Harmonic Acceleration (SHA) results. As the VOR gradually corrects for a vestibular insult, the phase abnormality and asymmetry begin to recover. Therefore, RCT is a good test to monitor the vestibular system over time. Other clinical applications may include assisting in diagnosing vestibular deficits that may be missed by caloric testing alone, confirmation of a suspected bilateral weakness, and monitoring the effectiveness of a treatment, such as chemical ablation or labyrinthectomy.
The three most common rotational chair tests are:
- Sinusoidal Harmonic Acceleration (SHA);
- Velocity Step Test (commonly referred to as “step rotation”); and
- Vestibulo-ocular Reflex (VOR) Suppression.
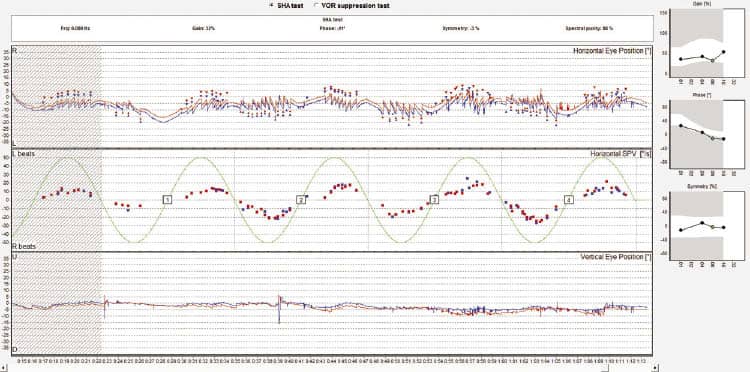
Sinusoidal Harmonic Acceleration. This test assesses the patient’s vestibulo-ocular reflex by rotating the patient in a pendular pattern at various frequencies from .01 Hz to .32 Hz (or higher) with vision denied. This test is the “gold standard” for identifying a bilateral vestibular weakness.11
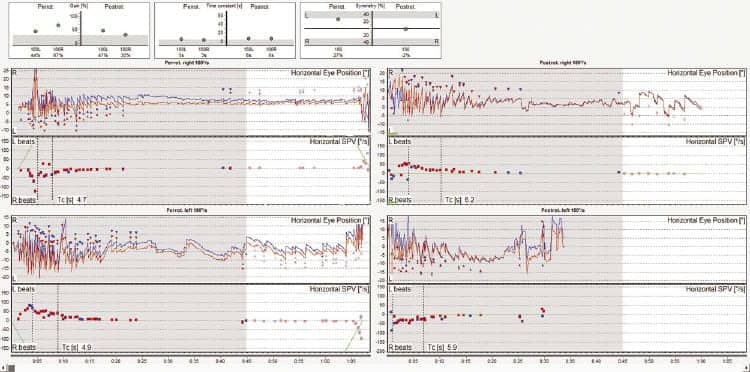
Due to nonlinearities of the anatomical vestibular system, assessment at multiple frequencies is recommended. Analysis parameters of particular interest with respect to SHA are gain (ratio of slow phase eye velocity to chair velocity), phase (timing relationship between stimulus and eye movement), and symmetry.12 When appropriately alerted, reduced gain is typically associated with peripheral vestibular pathology. Abnormal phase is associated with physiological damage to the patient’s VOR. Symmetry indicates the presence or absence of an imbalance in the system and can be used to help aid in determining which ear is weaker (Figures 7 and 8).

|
| Figure 7. Example of normal SHA result at .16 Hz. (Click to enlarge) |
|
| Figure 8. Example of borderline abnormal phase (°) across frequencies. (Click to enlarge) |
Velocity Step/Step Rotation. This test is used to assess the patient’s VOR by measuring the decay rate of nystagmus following an abrupt angular acceleration or deceleration to the right or the left (Figure 9).13 The most diagnostically significant parameter is the time constant. The time constant is defined as the amount of time it takes for the slow phase velocity of the nystagmus to decline by 37% of its peak velocity.
Reduced time constants may indicate either a unilateral or bilateral peripheral vestibular impairment, or a central vestibular pathology. It has been suggested that abnormally long time constants (Figure 10) may be correlated with motion intolerance or migraine-induced dizziness (see Jacobson & Shepard 2008, p 292).5
VOR Suppression. The purpose of the VOR Suppression Test is to assess the patient’s ability to suppress the VOR while rotating, similar to the Fixation Suppression test in caloric testing (Figure 11). Once the patient has been rotated at a specific frequency in SHA, the same frequency can be used to calculate a percentage of gain reduction to determine whether the patient can effectively suppress the VOR. A failure to sufficiently suppress the VOR can be indicative of possible central pathology.
Summary
This 3-part series of articles has explored and elaborated on the clinical usefulness and applicability of various tools and protocols for the evaluation and management of the vestibular patient. Part 1 offered 12 screening methods to quickly assess the dizzy patient without sophisticated equipment,14 and Part 2 explored the valuable contribution of videonystagmography to the evaluation of the dizzy patient.4
As noted in Part 1, efficiently and effectively diagnosing and treating dizziness is of paramount concern to the patient and the professional. Dizzy patients are among the most complicated and time-consuming patients seen in dispensing offices. Significant time commitments and expertise are required to obtain the case history and to document signs and symptoms, select and perform peripheral and central balance system tests, and more—all of which culminates in a comprehensive diagnosis, treatment plan, and even in-office therapeutic maneuvers.

|

|

|

|
| Tammy Bahner, MS, is a senior audiologist at Interacoustics USA in Eden Prairie, Minn, and Michelle Petrak, PhD, is director of clinical audiology at Interacoustics A/S in Assens, Denmark; Douglas L. Beck, AuD, is director of professional relations at Oticon Inc, Somerset, NJ; and Amanda Smith, AuD, is director of audiology at the private practice of Lakeside Physicians in Granbury, Tex. CORRESPONDENCE can be addressed to Dr Beck at: [email protected] | |||
References
1. Jacobson GP, Newman CW, Kartush JM. Handbook of Balance Function Testing. San Diego: Singular Publishing Group; 1997:157.
2. Barany R. New methods of examination of the semi-circular canals and their practical significance. Ann Otol Rhinol Otol. 1907;16:755-761.
3. Barin K. Interpretation and usefulness of caloric testing. In: Jacobson GP, Shepard NT, eds. Balance Function Assessment and Management. San Diego: Plural Publishing; 2008:230-252.
4. Smith A, Beck DL, Petrak M, Bahner C. In the trenches, Part 2: Videonystagmography (VNG). Hearing Review. 2012;19(12):12-24. Available at: /continuing-education/21284-in-the-trenches-part-2-videonystagmography-vng
5. Jacobson GP, Shepard NT. Balance Function Assessment and Management. San Diego: Plural Publishing; 2008.
6. American National Standards Institute (ANSI). ANSI/ASA S3.45-2009. Procedures for Testing Basic Vestibular Function. Washington, DC: ANSI; 2009.
7. McCaslin DL. Electronystagmography and Videonystagmography ENG/VNG. San Diego: Plural Publishing; 2012.
8. Melagrana A, D’Agostino R, Tarantino V, Taborelli G, Calevo MG. Monothermal air caloric test in children. Int J Ped Otorhinolaryngol. 2002;62(1):11-15.
9. Beck DL, Petrak MR, Bahner CL. Advances in vestibular diagnosis and rehabilitation. Hearing Review. 2010;17(11):12-16. Available at: /all-news/17030-advances-in-pediatric-vestibular-diagnosis-and-rehabilitation
10. Arriaga MA, Chen DA, Cenci KA. Rotational chair (ROTO) instead of electronystagmography (ENG) as the primary vestibular test. Otolaryngol Head Neck Surg. 2005;133(3):329-333.
11. Hain T. Meniere’s Disease; 2012. Available at: http://www.dizziness-and-balance.com/disorders/menieres/menieres.html
12. Valente ML. Adaptation of adult techniques for evaluating vestibular function in children. Hear Jour. 2007;60(10):34-44.
13. Brey RH, McPherson JL, Lynch RM. Technique, interpretation, and usefulness of whole body rotational testing. In: Jacobson GP, Shepard NT, eds. Balance Function Assessment and Management. San Diego: Plural Publishing; 2008:281-317.
14. Smith A, Petrak M, Bahner C, Beck DL. In the Trenches, Part 1: Screening tests for patients with dizziness. Twelve efficient screening methods for initial assessment of vestibular function. Hearing Review. 2012;19(4):12-23. /practice-management/17237-in-the-trenches-part-1-screening-tests-for-patients-with-dizziness
For further reading:
- Barin K. Background and technique of caloric testing. In: Jacobson GP, Shepard NT, eds. Balance Function Assessment and Management. San Diego: Plural Publishing; 2008:197-225.
- Cyr DG. Vestibular testing in children. Ann Otol Rhinol Laryngol. 1980;(Suppl 74, No 5, Pt 2):63-69.
- Jacobson GP, Newman CW. Background and technique of caloric testing. In: Jacobson GP, Newman CW, Kartush JM, eds. Handbook of Balance Function Testing. St Louis: Mosby Publishing; 1993:157-192.