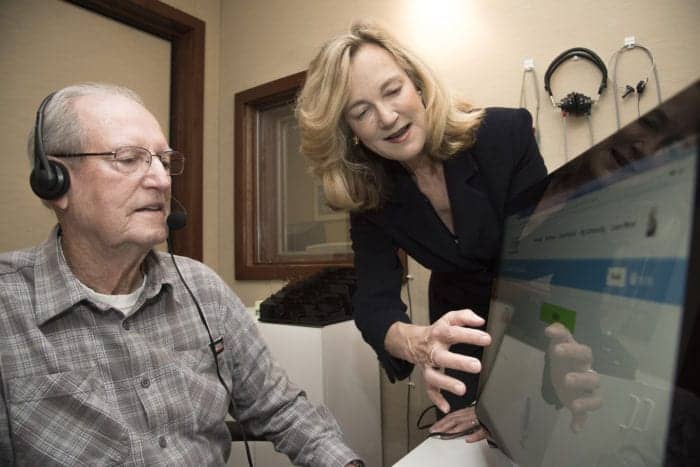
Nancy Tye-Murray, PhD, right, has developed training software to let patients with hearing loss practice listening to the voices they most want to hear. Tye-Murray helps Lonnie Willmann record audio clips for his wife, Kathleen Willmann, who has been diagnosed with hearing loss. Photo Credit: Robert Boston
By Julia Evangelou Strait
Hearing loss often is called the invisible disability, according to Washington University researcher Nancy Tye-Murray, PhD. It can masquerade as other problems, from dementia to depression, and it can make those problems worse. With an aging population, the detrimental effects of hearing loss will only grow.
To help people with hearing loss navigate their daily lives, Tye-Murray and her colleagues at Washington University School of Medicine in St Louis have developed software tools to improve speech recognition and to provide ongoing contact with an audiologist, the university announced on its website. The program is called “customized learning: Exercises for Aural Rehabilitation,” or clEAR. Working with Washington University’s Office of Technology Management, Tye-Murray and the program’s co-founder, Brent Spehar, PhD, a research scientist at the School of Medicine, launched a St Louis-based startup company in 2016 to provide the software to patients and hearing health-care professionals. Tye-Murray published an article about clEAR in the November 2016 edition of The Hearing Review.
“Hearing loss destroys self-identity,” said Tye-Murray, a professor of otolaryngology, and of audiology and communication sciences. “The inability to hear and participate in everyday conversations is isolating and can destroy relationships with family, friends, and co-workers. In my lab, we have been developing computer software to help adults and children with hearing loss practice listening, helping train the ear to better understand the people who are most important in their lives.”
In the U.S., more than 35 million adults report some amount of hearing loss, according to the Centers for Disease Control and Prevention. And more than a quarter of those over age 65 have what is considered disabling hearing loss, meaning they would benefit from hearing aids.

The clEAR software allows users to play computer games designed to be entertaining while letting them practice recognizing common words and sounds. It’s not the only such training tool available, but Tye-Murray said one of the aspects of this software that sets it apart from other programs is the ability to practice listening to specific voices.
“Our program includes traditional generic voices, but we also have a recording and editing system that lets patients train with the voices of people they most want to hear—often spouses, children, or grandchildren,” Tye-Murray said. “The patient’s spouse, for example, sits down and records the samples. Our software edits the audio clips. As soon as the recording is finished, the patient can begin training with his or her spouse’s voice.”
Tye-Murray’s research, published in the Journal of Speech, Language, and Hearing Research, has demonstrated that patients show improved recognition of a spouse’s speech when practicing with the spouse’s voice, compared with practicing with generic voices that are part of all other auditory training programs. That might seem intuitive, but historically, audiologists tended to assume that familiarity with a voice might limit the patient’s ability to further improve understanding of that same voice.
Tye-Murray’s work has shown that not to be the case. In particular, she said, the fact that the training is in the form of different games encourages patients to continue training to improve their scores. The program also is based on knowledge of cognitive psychology and how people learn a second language.
“We spend a lot of time training people to recognize words and sounds,” Tye-Murray said. “But we also train the cognitive skills necessary to understand speech, especially in environments with a lot of other sounds. These are skills like auditory attention, auditory working memory, and auditory processing speed.”
“Hearing aids don’t just amplify the voice you want to hear—they amplify everything,” she added. “They also don’t make up for the loss of specific frequencies of sound. So maybe a voice is louder, but it’s not necessarily clearer. You have to help patients interpret that distorted signal. This type of training helps people pull a single voice from the background noise of a crowded restaurant, for example.”
Another important aspect of the training that differs from other systems is that each patient works with an audiologist, who serves as a coach, monitoring the patient’s progress and encouraging him or her to continue training. Tye-Murray said her research shows that patients want to know that a professional cares that they are training, and they want the professional’s encouragement and structured guidance.
Tye-Murray emphasized that this training program can be used by anyone dealing with hearing loss, whether hearing aids, cochlear implants, or none of these tools are used.
“Some people with hearing loss don’t want to use these devices,” Tye-Murray said. “We want to make sure people know they can use this training program even without augmented hearing.
“Conversation is a cooperative effort—there are implicit rules that people follow when speaking with another person,” she added. “But when people have hearing loss, they break these implicit rules without realizing it. It may appear that they’re not paying attention, but the problem may be simply that they can’t hear what’s being said. They miss subtle cues, and that can make conversation difficult. We want to bring these problems into the light and talk about them, deal with them and come up with solutions that help patients communicate with the people who are most important in their daily lives.”