One of the great pitfalls of writing editorials for nearly 20 years—besides having a record in print of all the times you’ve been plainly wrong—is the same pitfall involved in aging or parenting: you run the risk of seriously repeating yourself. In truth, I could probably end this editorial by reprinting the September 2000 HR Staff Standpoint that details why affixing value for hearing services is important for at least three reasons:
- Consumers and third-party payors need to understand that the services provided by dispensing professionals are valuable and have real associated professional costs in both time and money.
- The inevitable popularity of the Internet and retail hearing aids will eventually produce consumers who need or demand a differing mix of professional services. This includes those people who have initially purchased a hearing device elsewhere.
- Fitting technology continues to progress to a point where first-fittings are “pretty darn good” fittings. But what remains is the assessment and individualization requirements associated with hearing aids that bring real value (and safety) to the products for consumers. These include but are not limited to verification/validation, counseling and rehab, post-fitting adjustments, etc (see the article, “The Secret Is Service,” by Jerry Northern, PhD, in the May 2012 HR).
Obviously, my editorial didn’t exactly make the field spin on a dime and abandon its tradition of bundled pricing. But I’m in pretty good company. For example, George Osborne, PhD, wrote in a March 1995 HR article titled “How to Determine Pricing for Hearing Care Services” that:
We are professionals and business people. The audiology community is slowly coming to realize that the business-aspect of a hearing care office can be almost as important as the skills of the people who practice there. There are many fine offices and practices that have closed their doors because the manager and/or professionals who work there couldn’t understand that they contribute to a business. No matter how idealistic you may be, reality dictates that an office/practice that goes out of business cannot help anyone.
A second paradox also exists for hearing care professionals, and it has to do with the very words “professional” and “professionalism.” Too often, the people in our field blush or become sheepish when charging for services rendered. Some private practices don’t charge anything for audiometric services as long as the client purchases a hearing instrument [Dr Osborne included a table that compared 1995 medical pricing ranging from $65 for a hearing aid check to $396 for an audiological assessment in medical settings versus $0 for the same services in private practice settings]. This is, quite frankly, ridiculous. Hospitals and medical clinics charge for audiological services. And they should; it costs them substantial amounts of money to provide those services.
Not charging for services may also be sending a dangerous message that could be misinterpreted by government regulatory agencies and/or those formulating future healthcare guidelines. We must unbundle our fees….Our profession needs to demonstrate clearly that hearing screenings, audiometric assessments, hearing aid evaluations, and follow-up re-evaluations are not “free” or “throw-in” services. Keep in mind that this discussion does not even consider the fact that professionals spend generous amounts of time and money and sweat in educating themselves. Not charging for services denigrates all qualified professionals, and it poses a serious threat to the profession’s autonomy.
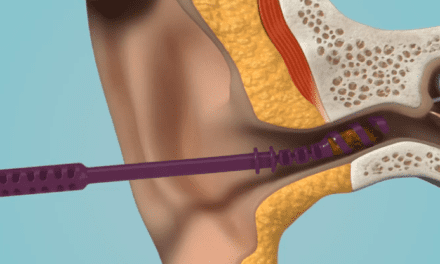
I am aware of the practical reasons why the majority of professionals continue to bundle their pricing. But I also believe that the points detailed above are more important today than they were in 1995 or 2000. Our field is evolving rapidly, as evidenced by this month’s 3D ear scanning technology article and an upcoming HR editorial package on tele-audiology guest-edited by Dr Northern this fall.
There are unbundled models in the field that work, including those presented recently by the folks at the University of North Carolina-Chapel Hill and elsewhere. Hearing care professionals should continue to examine these and see how they might fit into their business models.
Karl Strom
Editor-in-Chief