People with tinnitus often characterize their tinnitus as “ringing in the ears” or a “buzzing sound.” The American Tinnitus Association (ATA) describes it as a subjective noise that only the patient can hear. In some cases of objective tinnitus, physicians can identify the symptom with the use of a stethoscope placed on the neck or directly in the ear canal.
About 50 million people in the United States experience tinnitus to some degree and, in severe cases, seek medical attention. There is currently no known cure for tinnitus; however, there are advanced devices and treatments today that can help alleviate tinnitus symptoms.
The Hearing Review takes a closer look at tinnitus treatment by interviewing three audiologists who are associated with GN Otometrics and Audiology Systems: Clément Sanchez, AuD, product manager at Otometrics; Wendy Switalski, AuD, audiology development manager at Audiology Systems; and Clint Keifer, AuD, audiologist at Great Lakes Audiology. Drs Sanchez, Switalski, and Keifer share their thoughts on the benefits of tinnitus assessment, and provide advice to audiologists and hearing care professionals who are interested in adding tinnitus assessment to their practice.
HR: Why should hearing care professionals who traditionally focus on hearing impairment get involved in tinnitus?
Clint Keifer, AuD: As audiologists, we possess an in-depth understanding of the anatomical, physiological, and psychoacoustical aspects of the auditory system. As hearing care professionals, we are skilled in diagnostic, counseling, and rehabilitative approaches to managing auditory disorders. With this clinical foundation, few other health professionals are as well suited to help those with tinnitus. Good tinnitus resources are needed in every community to bring new exposure and business to your office.
Wendy Switalski, AuD: In conversations I’ve had as an audiologist and as a consultant to audiologists, it is clear that these conditions coexist for so many of our patients. And for some of them, treating the tinnitus is necessary to address the concerns that led them to seek hearing care in the first place.
Clement Sanchez, AuD: Tinnitus can be a problem for those who are hearing impaired and have a hearing loss. Tinnitus can also be a problem for those with only some degree of hearing loss. For example, the US Center for Health Statistics estimates that tinnitus was reported by 25% of those who are hearing impaired and have hearing loss. The Tinnitus Clinic at Oregon Health and Science University found that 90% of their patients who have tinnitus also have some degree of hearing loss.
Tinnitus can have a dramatic effect on the lives of these patients. They may have difficulty sleeping, be unable to concentrate, and experience irritability and high stress levels. The hearing care professional needs to consider these issues if they want to succeed in managing the hearing loss on top of the tinnitus.
HR: How effective are hearing aids at solving tinnitus problems? Does this always entail special masking? What other devices are available and recommended for tinnitus patients?
Sanchez: Hearing aids can be very effective if they can reduce the symptoms related to the tinnitus. A hearing aid can amplify soft sounds, which can have a “masking” effect and helps to decrease the contrast between the environmental sounds and the tinnitus. However, it’s important to check the effect of the external sound on the tinnitus before introducing the benefits of wearing a hearing aid to the patient.
Therefore, before choosing a device, I recommend patient counseling and assessment. This is an important step to address the patient’s fears and provide supportive tools when the tinnitus is too intense.
A clinician can play a vital role in helping the patient deal with the sounds of everyday living, instead of avoiding sounds all together. Today, tinnitus management tools also include sound enrichment devices, sound generation pillows, as well as sound generators like MP3 and relaxing music.
HR: What is the best way for a clinician who to add tinnitus treatment? Are there different levels at which practices can participate, or should every hearing care practice seek to have a full-service tinnitus treatment plan?
Switalski: Professionals interested in expanding their services have so many resources available. These include seminars, online training, textbooks, and articles. Additionally, training from hearing instrument manufacturers and collaborating with colleagues can be valuable.
Practices may begin by simply offering tinnitus assessment, patient questionnaires, or surveys. They can also provide informational counseling and supplement their fittings with hearing instruments that include features and options for tinnitus relief.
Keifer: Ideally, practices would be “full-service,” but in practical terms, it is difficult for any one practice to offer every possible solution. My recommendation would be to offer as many options as possible within the means of the practice and the practitioner. Then be sure to include information that the patient may benefit from—like additional options or resources not offered at your practice.
Sanchez: Assessing tinnitus can be challenging, so clinicians who decide to add a full-service tinnitus treatment plan have a few details to consider. Collaboration with other professionals like ENTs, psychologists, and general practitioners is helpful. It is important to consider that treating patients with tinnitus requires the ability to listen and a high degree of patience. In some instances, testing procedures may take time. For example, a clinician may have to wait for the patient to fall asleep using a sound generator pillow.
Aside from my traditional practice, I used to schedule consultation with tinnitus patients 1 day a week and this worked well. Tinnitus consultation can overlap with hearing loss management and counseling. When testing patients with tinnitus, clinicians should consider scheduling a dedicated time just for consultation because it will take longer than usual and the patient is expecting a solution.
HR: I’ve heard that tinnitus patients can consume huge amounts of practice time and many dispensing professionals are not adequately staffed for that. So, what are the practical options?
Sanchez: Yes, tinnitus patients will need time to express their fears, frustrations, and the discomfort they are experiencing because the sounds they hear are unclear and can be difficult to describe. Establishing a road map with the patient is also necessary. For this, I would recommend using an analog visual scale of relief to set the objective from the very beginning.
I would describe the tinnitus consultation as “a mix of charisma and empathy,” where clinicians can focus on gathering the information that can benefit the treatment. Empathetic listening is best for a successful tinnitus consultation. When the patient becomes more comfortable describing their situation, the clinician should then begin to drive the conversation. This typically happens during the first appointment and can take up to 1 hour.

The MADSEN Astera2 features a dedicated tinnitus assessment module designed to help clinicians address increased claims for tinnitus and hearing loss disability.
The new tinnitus test module we have developed as part of fundamental audiometry in MADSEN Astera2 supports the professional through a series of integrated questionnaires. Prior to the consultation, patients can fill out questionnaires in the waiting room to avoid external influences during the test. Then the follow-up treatment can be done online, where the answers provided previously can help clinicians evaluate the impact of this strategy.
HR: What is involved in a tinnitus treatment protocol?
Keifer: Tinnitus treatment protocols should not be rigid, but rather they should adapt to the individual. While proper diagnostic testing and quantification measures should be performed for hearing and tinnitus aspects, the treatment options will vary greatly based on the individual and should focus on addressing identifiable needs. This may include education, information, or recommendations for further medical evaluation or treatment by other professionals.
The treatment may also involve retraining strategies, amplification, masking, sound therapy device application, support group attendance, and so forth. Tinnitus can be viewed as a spectrum disorder where trying a combination of approaches may be necessary.

A closer look at the tinnitus module integrated within MADSEN Astera2 and OTOsuite™. Highlighted in magnifying glass on lower left is the electronic questionnaires for the TFI, THI, and Tinnitus and Hearing Survey (THS), which saves in NOAH and eliminates the need for paper records.
Sanchez: In addition, it will entail an in-depth hearing assessment, such as audiometry with UCL, immittance, otoacoustic emissions (OAE), and auditory brainstem response (ABR). Clinicians should ensure they are working with a subjective tinnitus and characterization via the existing questionnaires, like the Tinnitus Handicap Inventory (THI), Tinnitus Functional Index (TFI), and Tinnitus Handicap Questionnaire (THQ). Psychoacoustical tests are also important and can include pitch and loudness matching and minimum masking level (MML). All these tests provide an excellent basis and a good start for constructive dialogue.

The full tinnitus psychoacoustic test battery is designed to improve patient counseling and test precision. Testing efficiency and immediate availability of measurement results allow more time for consultation.
Visualization of the tinnitus on the audiogram is a great experience for a patient who has looked for help for years and may have felt misunderstood at times. Having a picture of this “phantom pain” helps both clinician and patient communicate about “pain relief.”
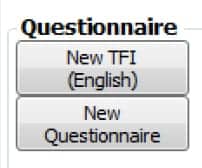
The electronic questionnaires—Tinnitus Functional Index (TFI), Tinnitus Handicap Inventory (THI) and Tinnitus and Hearing Survey (THS)—can be saved in NOAH and are designed to eliminate the need for paper records.
The next step is explaining that, for example, a 7 dB tinnitus is quite a small issue that can be managed. Test results will provide the professional with information concerning the effect of an external sound on the tinnitus. If there is a positive impact, like an attenuation of the perception, a strategy like the TRT (Tinnitus Retraining Therapy) can be considered.
Once again, dialogue with other professionals is important and should be considered from the very beginning. Psychological or a drug support can be helpful in parallel.
HR: What types of equipment should you consider for your practice when starting up a tinnitus treatment program?
Switalski: Having access to the proper audiometer features is important for performing a tinnitus assessment. This includes options for changing intensity, step size, and frequency resolution. Additional helpful information may be gained from high frequency audiometry and OAE.
Sanchez: Clinicians can start by investing in a full-featured clinical audiometer. A high-resolution audiometer in frequency (1 Hz) and intensity (1 dB) is required to perform a characterization of the tinnitus. The validated questionnaires, integrated or paper, are necessary as well. If the patient can accept a sound generating strategy, many hearing instrument manufacturers deliver interesting solutions today—with or without an amplifier for the hearing loss.
Otometrics has developed a dedicated tinnitus management tool for audiologists, which is integrated with our clinical audiometer, the MADSEN Astera2. Today’s clinicians and audiologists can now more effectively evaluate the tinnitus and its impact on the lives of their patients.
CORRESPONDENCE can be addressed to Dr Switalski at: [email protected]. More information can be found at: www.audiologysystems.com/tinnitus








