There is significant multidisciplinary interest in modifying risk factors for falling in the population of older adults.
Patient Care | March 2023 Hearing Review
By Joseph Sakumura, AuD & Richard Gans, PhD
Introduction
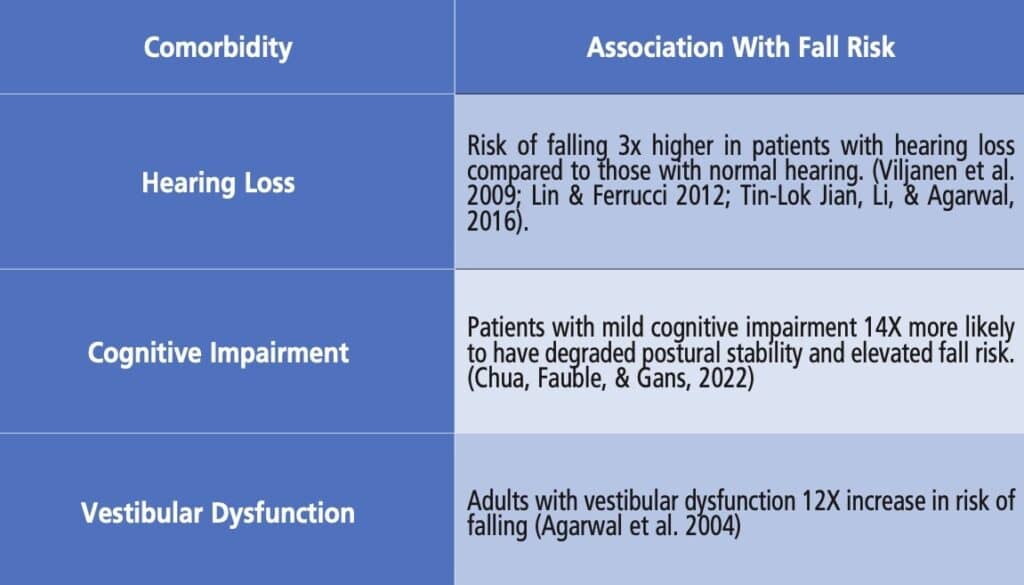
Falls are the leading cause of fatal and non-fatal injuries for Americans, often leading to loss of independence and quality of life. One-third of older adults fall annually, creating a significant strain on the medical economic system of the United States and costing an estimated 34 billion dollars annually to cover direct medical expenses and hospitalizations.1 This has led to a significant multidisciplinary interest in modifying risk factors for falling in the population of older adults. The association between hearing loss, vestibular dysfunction, and cognitive impairment and how each contributes to imbalance and elevated fall risk have been well documented in the literature. Figure 1 summarizes the findings and the association between these comorbidities and falls. The specialties of audiology and otolaryngology are often the most sought-after specialists for patients with complaints of audio-vestibular dysfunction. Recent investigators2 have published the relationship between cognitive dysfunction, elevated postural instability, and fall risk.
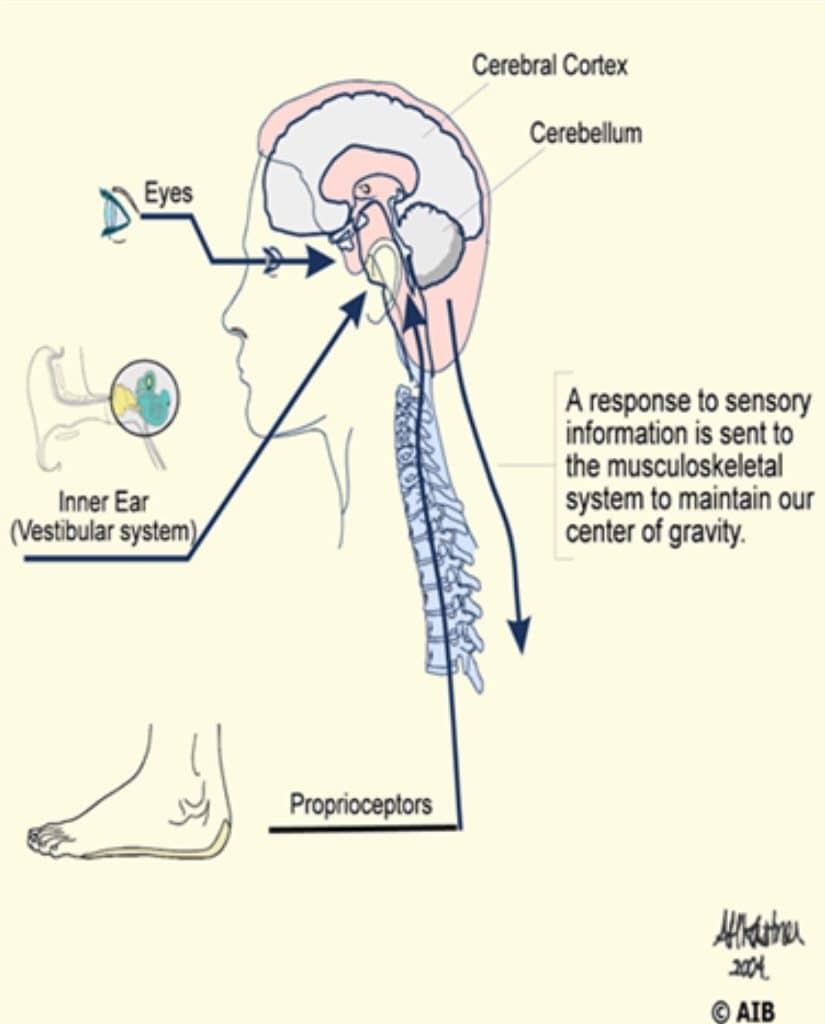
Human equilibrium is a complex process involving peripheral sensory modalities and the central nervous system. Figure 2 is a schematic of postural control in humans. Modern equilibrium theory recognizes the contribution and interaction of the vestibular, visual, and proprioceptive mechanisms. While the role of these three sensory modalities is well understood, recent scientific literature and clinical findings suggest auditory function also plays a large role in maintaining balance and mitigating fall risk.3-5
The impact of untreated hearing loss on cognitive function is well documented in the literature, and hearing loss is recognized as the number one modifiable risk factor for cognitive decline. Furthermore, patients with even mild cognitive impairment in domains of: visuo-spatial processing, executive function, memory recall, and reaction times are 14 times more likely to have degraded postural stability and elevated fall risk.6 It is estimated that the vestibular system is responsible for at least 85% of the sensory information required to maintain normal equilibrium. Therefore, even minor vestibular dysfunction will significantly increase fall risk.7 If there are additional comorbidities affecting vision or somatosensory function, as is common in the older population, e.g., peripheral neuropathy, glaucoma, and retinopathy, the risk is amplified.
Comprehensive Evaluation Protocols
Having an established framework for the interaction between these sensory modalities and their impact on cognition is important in managing fall risk. Patients presenting to providers with generic complaints of imbalance, recent falls, or dizziness should undergo postural stability testing, comprehensive neurodiagnostic evaluation of the audio-vestibular system, and cognitive screening as the first step of a fall risk management program.
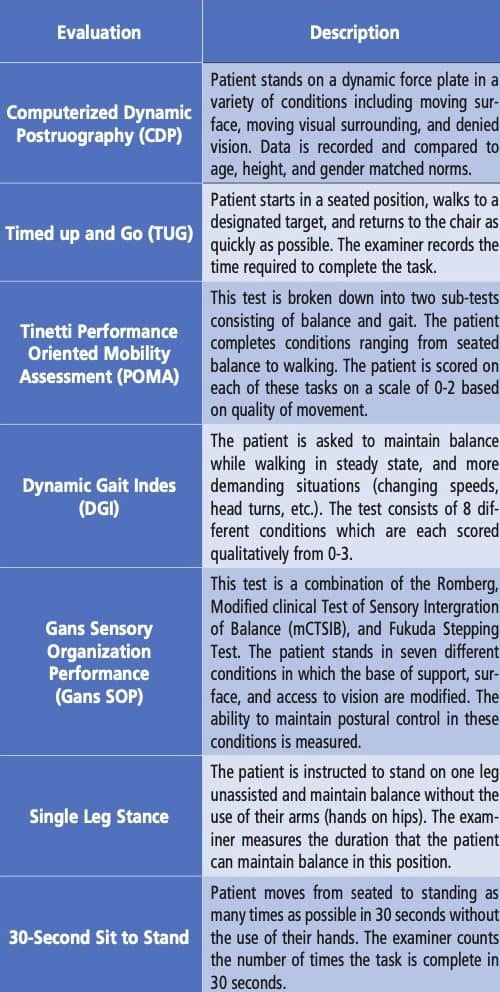
Evaluation of these patients may be influenced by access to instrumentation and clinical experience but should be as thorough as possible. A comprehensive case history is mandatory. Questions should include; a history of falls, where they occurred inside the home or away, near falls, and any fear of falling. Fall risk assessment should include a standardized test of postural stability to evaluate global equilibrium function. This may be completed with technology (e.g., computerized dynamic posturography, force plate, etc.) or at the bedside with validated protocols (e.g., Gans SOP, TUG, POMA, Single Leg Stance, Tinetti, etc.). For a summary of available postural stability, tests see Figure 3.
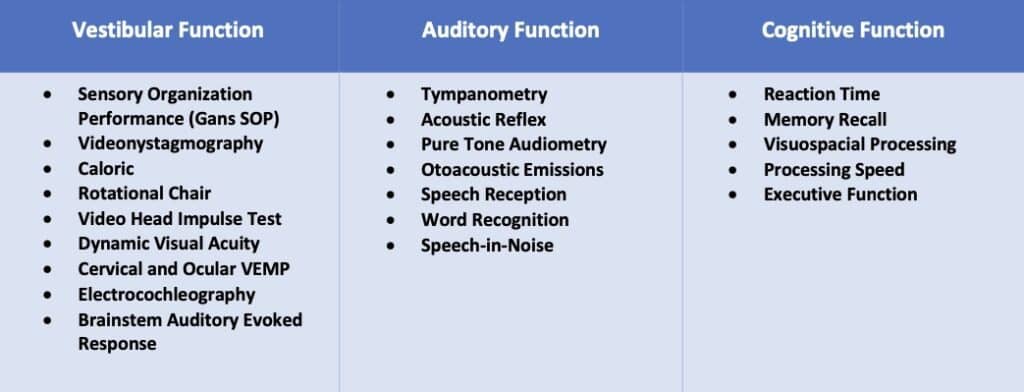
Neurodiagnostic evaluation of the audio-vestibular system should include protocols that identify the nature of involvement and guide treatment recommendations. Likewise, cognitive screening should be performed with standardized protocols in the cognitive domains involved in balance function (reaction time, processing speed, memory recall, executive function, etc.).
Traditionally, cognitive function tests have been administered in paper and pencil format. These have included Montreal Cognitive Assessment (MoCA) and Saint Louis University Mental Status Exam (SLUMS). Recently, an FDA cleared computer-based cognitive screening tool, Cognivue Thrive, has gained attention as an effective, easy, fast, and standardized tool for use by audiology and ENT practices.
CognivueTM is an effective and efficient screening tool, however pen and paper tests (e.g., MoCA, SLUMS, etc.) also exist. Figure 4 outlines an example of a comprehensive evaluation protocol for vestibular, auditory, and cognitive function.
Diagnosis-Based Strategies of Management
Following a comprehensive evaluation of the contributory balance function systems, a fall risk profile may be developed, followed by intervention and management recommendations. Patients should be counseled on results and educated on fall risk management. Written and verbal format is recommended with specific instructions on safety both inside and outside of the home (e.g., footwear, night lights, uneven surfaces, rugs, assistive devices, etc.). Based on the patient’s age, living arrangements, socioeconomic status, and cognitive function, family or caregivers should be encouraged to participate in the counseling. The finding and recommendations should also be communicated with the referring physician. The patient’s primary or referring physician may know the patient well and have a long-time relationship. Their participation in the patient’s plan of care will greatly influence the patient’s compliance.
Conditions identified during the evaluation may be best addressed through a diagnosis-based strategy approach. Is the patient’s elevated fall risk due to an easily treated BPPV or do they present with cognitive decline, bilateral vestibular hypofunction, orthopedic, and or vision comorbidities? The more complex the patient’s conditions, the more team members may be necessary. The goal is to maintain the patient’s safety and their ability to age in place and live independently.
Patients with hearing loss should be counseled about the effect of untreated hearing loss on postural stability and the increased fall risk, even in individuals as young as 40 years of age.7
These patients will require an interdisciplinary approach to management. Biomechanical or neurologic involvement which includes; orthopedic conditions, neuropathy, Parkinson’s, or just deconditioning, which is best managed by physical therapists with specialized training or certification. Balance retraining therapy should be encouraged for patients at elevated fall risk with protocols including; strengthening and conditioning, recovery strategies, activities of daily living, and assistive device use.
Cognitive impairment identified through screening should be discussed with the referring physician and addressed by the appropriate team, often comprised of; psychology, neurology, speech-language pathology, or occupational therapy. As cognitive impairment is associated with elevated fall risk, and hearing loss has been identified as a modifiable risk factor for cognitive decline, immediate treatment with amplification should be strongly recommended for patients with hearing loss and cognitive impairment.2
The following case study outlines a clinical pathway for evaluation and management recommendations for a patient presenting with recent falls and complaints of dizziness.
Case Study
History
A 67-year-old female presents to the clinic with primary complaints of dizziness and imbalance. She remarks on an imbalance that has been progressively worsening over the last year and that about two months ago, she had an attack of vertigo lasting a few hours. Since then, she has experienced oscillopsia, and head movement provoked dizziness. She reports her balance function has worsened significantly. In the last month, she has fallen twice outside of her home while shopping, neither of which resulted in significant injury. She has also developed a more sedentary lifestyle due to fear of falls and return of a vertigo episode. She has never been to physical therapy and says she is “very careful when walking.” The patient denies any change in hearing but states for years she has had difficulty hearing in noisy restaurants. Medical history is remarkable for type 2 diabetes and neuropathy in both feet. She wears glasses, and has had a recent optometric examination but does report diabetic related retinopathy, worse in her left eye.
Examination
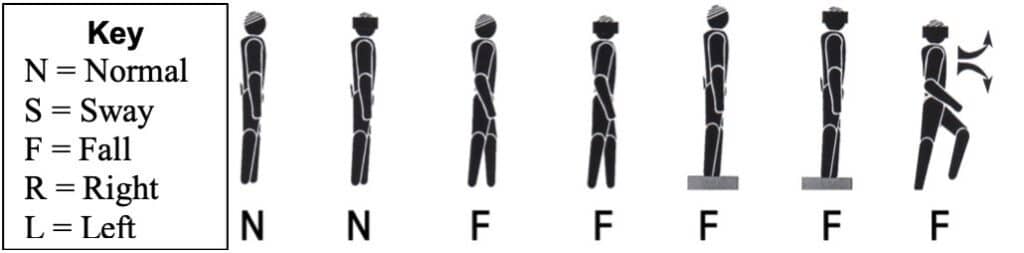
Postural stability testing was completed with the Gans Sensory Organization Performance (SOP). The patient’s pattern of postural stability was consistent with a multifactorial disequilibrium. SOP testing was indicative of grossly degraded balance function and elevated fall risk. Figure 5 shows the patient’s performance on the SOP.
Audiometric studies were completed and revealed a mid to high frequency moderately severe sensorineural hearing loss. Middle ear function was intact and hearing thresholds were symmetrical.
Neurodiagnostic evaluation of vestibular function revealed a non-compensated left peripheral vestibular hypofunction. This was evidenced by reduced VOR gain in response to bilateral bithermal caloric air irrigations and the corresponding patterns of abnormality with rotational chair, vHIT, and VEMP studies.
Cognitive screening was completed using the CognivueTM Thrive screening protocol. The patient scored in the moderate range for both memory (MEM) and visuospatial (VSP) domains and poor for reaction time (RT), processing speed (PS), and executive function (EF).
Recommendations
Given the multifactorial nature of involvement the patient was counseled extensively on findings and the following multidisciplinary treatment plan was discussed:
1. Follow-up visit with an audiologist to discuss amplification as management of the identified hearing loss. Although her primary functional impairment was not hearing difficulty, the patient was educated on the role of untreated hearing loss in cognitive and equilibrium function. She ultimately moved forward with the recommended amplification treatment plan.
2. Recommended hybrid protocols of vestibular and balance rehabilitation therapy with an American Institute of Balance certified physical therapist. As neurodiagnostic evaluation identified a non-compensated left vestibular hypofunction, ideal protocols would include gaze stabilization, adaptation, habituation, and substitution to facilitate compensation. Additionally, balance retraining protocols of strengthening and conditioning, recovery strategies, activities of daily living, and fall risk management would be beneficial. All protocols should be completed with tasks of executive function.
3. Abnormal Cognivue scores were discussed with the patient and her referring physician, who ultimately recommended consultation with neurology/neuropsychology.
4. Finally, the patient was counseled extensively on fall risk management and safety both inside the home and out. Information was provided in a both written and verbal format and received well by both the patient and her spouse.
Summary
Balance function is a complex process. Normal balance function requires intact sensory input from multiple peripheral sensory systems and an intact central nervous system. The assessment of each sensory system and their integration into the totality of the individual’s postural stability in static and dynamic conditions will provide the most predictive evaluation. This may be accomplished with standardized screening protocols or comprehensive neurodiagnostic vestibular testing, if available. Numerous investigators and clinicians are now stressing the inclusion of cognitive screening as an important component in fall risk assessment. The cognitive overload of attending to a highly dynamic world for individuals with hearing loss, vestibular dysfunction, and cognitive decline increases the likelihood of a fall. An individualized intervention and management Plan of Care with appropriate practitioner team members will provide the patient with the best therapy outcomes, reduce the likelihood of a fall, and improve their quality of life.
Citation for this article: Sakumura J, Gans, R. Fall Risk Management in Audiology and ENT Practice: The Role of Cognitive, Vestibular, and Auditory Function. Hearing Review. 2023;30(3):16-20.
References:
- Kowalewski V. Hearing loss contributes to balance difficulties in both younger and older adults. Journal of Preventive Medicine. 2018.
- Chua K, Gans RE, Fauble BM. Association of cognitive impairment and fall risk in older adults: an analytical cross-sectional study. Journal of Otolaryngology-ENT Research. 2022;4(1)8–12.
- Jiam NTL, Li C, Agrawal Y. Hearing loss and falls: a systematic review and meta-analysis. The Laryngoscope. 2016;126(11)2587–2596.
- Carpenter MG, Campos JL. The effects of hearing loss on balance: a critical review. Ear & Hearing. 2020;(41).
- Goman AM, Lin FR (2018). Hearing loss in older adults – from epidemiological insights to national initiatives. Hearing Research. 2018;(369)29–32.
- Agrawal Y, Carey JP, Della Santina CC, et al. Disorders of balance and vestibular function in US adults. Archives of Internal Medicine. 2009;169(10)938.
- Rumalla K, Karim AM, Hullar TE. The effect of hearing aids on postural stability. The Laryngoscope. 2014;125(3), 720–723.