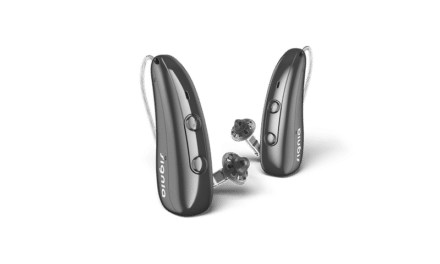
Featured image: Dr Beck wearing his right and left Starkey Genesis IIC. People with less than 70 dB of hearing loss (it varies with canal size, hearing loss configuration, and more) can often wear cosmetically “less challenging” canal aids or essentially invisible-in-the-canal custom-made devices. Photo: Beck
If patients don’t want to wear obvious hearing devices because of perceived stigma, let’s give them the option they do want.
By Douglas L. Beck, AuD; and Michael A. Harvey, PhD
Age-related hearing loss (ARHL) is nothing to be ashamed of. Nor is hip replacement, knee replacement, osteoarthritis, diabetes, cardiovascular disease, dental implants, or cosmetic surgery. These are often simply the results of time acting upon the human body. Time and gravity always win. This is aging—which ain’t always pretty.
However, we should acknowledge that many (probably most!) people do not care to share, show, or talk about their age-related deficits, problems, or disabilities. Millions of people get their teeth straightened using Invisalign (and similar) as it allows correction and it is more-or-less invisible. Hundreds of millions of people in the U.S. wear contact lenses; receive LASER eye correction surgery; wear wigs and toupees; wear hair extensions; get hair transplants; get all manner of implants; wear make-up; get Botox, as well as facials, chemical peels, and other skin treatments, and more. These are essentially personal decisions made to make the individual feel better about the way they perceive their own physical appearance. Adults making personal decisions, that is fine.
However, in hearing healthcare we often hear versions of “We should not encourage people to hide their hearing loss;” after all, “Hearing aids aren’t as visible as your hearing loss…” and, “By wearing and promoting tiny (nearly) invisible hearing aids, you’re implying that people should be ashamed of their hearing loss and hearing aids and these things should be hidden.” Respectfully, we are having none of that. We are simply pro-choice. We believe adults should be aware of, should be knowledgeable, and should be able to choose options and solutions for themselves as they see fit. It is their choice and it’s none of our business.
As Harvey notes in his 2023 article “Aging with Dignity with Assistance From an Audiologist,”(1) one facet of “aging with dignity” involves self-agency, which can be defined as one’s right and ability to make choices. Perhaps Descartes should have said “I decide, therefore I am.” In other words, how we appear matters to most of us. Many (if not most) do what they can to look as vibrant, young, and healthy as they can. Very few people try to intentionally look older, less competent, or disabled.
Sadly, it is well known that most people who would benefit from hearing aids do not use them, even though Kochkin & Rogin(2) noted professionally fitted, programmed, and dispensed hearing aids help one to be more socially active; more communicative; and more engaged in social, business, recreational, and personal matters. They reported hearing aids help reduce anxiety and depression and help us communicate, yet, most people are not willing to wear them. Period. One out of five people in the USA has hearing loss and only 10% of them wear hearing aids.(3) Houston, we have a problem
Of course, some people may make the argument that access and affordability were/are the major stumbling blocks to acquisition. However, although access and affordability are very important, there appears to be another major reason people do not generally seek hearing aids. Specifically, the long-held, well-documented hearing aid stigma is alive and thriving. One might define hearing aid stigma as the perception that hearing aids are a visual distraction which are generally considered not physically attractive, and the perception is (see the references below) that hearing aids make the wearer look older, less competent, and/or less intelligent.
Hearing Aid Stigma
There is ample evidence of stigma associated with both old age and hearing aids in our culture from long ago through to 2024.
Capitalizing on the quest to look younger, companies present a plethora of billboards for “age-defying” skin treatments and late-night ads for local plastic surgeons jabber on and on about wrinkles like they were generals describing hostile enemy forces, reports Levy.(4)
Amlani(5) reports that even if hearing aids were given away free, two-thirds of the hearing-impaired population would not bother to acquire hearing aids.
Wallhagen(6) reports pervasive perceived stigma associated with hearing loss and hearing aids and the close association with ageism and perceptions of disability. She notes young adults report the negative impact of hearing loss and hearing aids on their relationship with peers, self-concept, and willingness to self-disclose.
People with hearing loss avoid hearing aids for many reasons and “social stigma” plays a significant role, according to a 2024 Forbes survey.(7) In the survey they report 48% of respondents believe there is a stigma associated with hearing aids. They report 63% of Millennials, 47% of Gen Xers, and 41% of Boomers agree, there is a stigma.
WebMD(8) says essentially the same thing: 62% of Americans wear visible corrective eyewear and 45 million wear contact lenses. Yet, only 15% of people with hearing loss wear hearing aids. They report resistance to hearing aids is deeply rooted in stigma, specifically with old age.
Beadle, Jenstad, et al(9) report younger and older adults might hold negative implicit attitudes toward older and younger people who wear hearing aids.
A study by Nickbakht, Ekberg, Waite, et al(10) explored how and when a stigma-induced identity threat is experienced by adults with hearing loss and their family members. They report all participants in their study believed hearing loss and hearing aids were associated with stigma. They also report an association between hearing loss and hearing aids and stereotypes associated with aging, disability, and difference; and more.
Rather than denying the persistence of the hearing aid stigma, we, the authors, are admitting it and we are trying to accommodate and facilitate a more-willful desire to acquire and wear hearing aids and to increase patient adherence, if clinically appropriate. Certainly, custom-made products are not appropriate for all situations.
Patient-Centric Perspective
The FDA was tasked with creating OTC to provide more affordability and access to hearing aids, rather than providing hearing healthcare or professional hearing services to educate, counsel, diagnose, and guide the consumer. They do not have to be mutually exclusive. In fact, the FDA eliminated the hearing care professional from the equation for OTC patients. The FDA missed the obvious and they doubled down on the ridiculous. We are not opposed to OTC. Not at all. Patients are allowed to choose OTC; they have the right to choose OTC; OTC makes absolute sense.
However, the FDA could have done a much better job by simply recommending or mandating (their choice) a comprehensive audiometric evaluation by a licensed hearing healthcare professional to facilitate a diagnosis and to offer education, guidance, and counseling, and then allow the patient to make up their own mind about what to buy and where and how to buy it. Some might opt for OTC, perhaps others would select prescription products. Either would be fine. It would be a personal choice as to what to buy and where to buy it. We will never know how well OTC might have gone had FDA required the time-honored medical protocol of “diagnosis first, treatment second.”
That ship has sailed.
As professionals, we can continue to promote highly visible hearing aids that people typically do not want to wear or, moving forward, we can revive a previously successful patient-centric perspective.
Permit us to offer an analogy.
A child was learning how to become a baseball umpire. Three umpires gave their advice. The first umpire said, “I call them as I see them.” The second umpire said, “I call them as they are.” The third umpire said, “They are as I see them.”
Most people are the “third umpire.” They construct their own reality and they perceive visible hearing aids as stigmatizing. The failure to attract people with hearing loss to hearing aids has a lot to do with the individual’s preference and choice to not broadcast or advertise their personal problems, issues, or disabilities, etc. These are individual choices and very much no one else’s business, unless the adult chooses to share it.
Custom-made nearly invisible products are generally not available via OTC, or big-box, or online resources because “customs” require more professional skill, knowledge, expertise, patience, and often, artistic ability, too. Creating custom products in the manufacturer’s lab is difficult and requires extraordinary skill, expense, tools, machinery, knowledge, and patience. However, some people will prefer and choose instant-fit on-the-shelf products with tulip-domes and that, too, is their choice. For people with more significant hearing and listening needs, the best choice may be RICs, RITEs, or BTEs to accommodate space occupying features (beamformers, T-coils, Bluetooth, etc.) with a custom earmold, but again, personal choice.
Benefits of Custom Products
In my case (DLB), despite ridiculously small ear canals and despite an unusual sensorineural hearing loss, I would not choose visible BTEs or mini-RITES for me. I have chosen Starkey Genesis custom-fit IICs. I choose to keep my hearing and listening issues essentially out of sight. We believe most people with mild-to-moderate hearing loss would make a similar decision if given the choice, and if that option is clinically appropriate. For some people, wearing custom-made IICs (and other custom-made nearly invisible products) removes the hearing aid stigma from the equation, thereby allowing a more palatable choice for the patient.
Contemporary high-resolution and high-illumination video-otoscopes offer a significantly improved and safer custom products protocol. Acquiring a deep canal impression (past the second bend) is arguably safer and easier than ever before. Likewise, the hearing aid technology we have in 2024 is tremendously improved from the custom products from a decade ago.
Of note, when fitting and programming deep fitting devices, progressively less gain is required as the medial tip of the hearing aid approaches the tympanic membrane (TM) and as the cavity between the hearing aid and the TM decreases. Appropriate venting can be used to decrease the sensation of “own voice” if needed, and appropriate venting allows more of the sound to be processed (i.e. better noise reduction) through the sophisticated hearing aid circuit as compared to a mini-rite with a “tulip dome,” which allows unprocessed sound to pass directly to the tympanic membrane, without maximal benefit of high-tech directionality or noise reduction. The fixed location of a recessed faceplate within the canal allows improved natural directionality as the anatomy of the ear facilitates this.
It has been obvious to many of us for decades that dome-fittings of mini-RITEs and RICS and many BTEs are generally not properly aligned on the horizontal azimuth. They are often worn pointed upward, thereby allowing less-than-optimal (or anticipated) directional or amplification benefit. Custom earmolds and custom hearing aids help provide and ensure a correct horizontal placement.
OTC Affordability and Accessibility?
Two years after the FDA allowed OTC, we observe that “access” appears to have been increased. However, the better OTC products often cost $1,000 to $2,950 per pair(11), placing the better OTCs beyond the reach of most of the people OTC was created to help. Sieber reports that at Best Buy, OTC products range (per pair) from $200 to $2,550.(12) Suzy Orman reports that most Americans (60%) do not have $500 for an emergency.(13) As such, it seems hard to imagine that most Americans could spend more than $500 on a pair of low- to mid-range OTC hearing aids.
Custom-made products are not available as inexpensive mass-market products and they require more time, labor, and expertise from the hearing care professional and the laboratory, and custom products may cost more. However, for the price of premium OTCs, prescription mini-RITES, and similar form factors, quite often, custom-made products are available and offer multiple benefits (as detailed above).
For those with financial challenges there are modern payment solutions used in dentistry, surgery, medicine, plastic surgery, and other healthcare choices and needs. For example, CareCredit offers a health and wellness credit card that empowers and enables patients to receive optimal dentistry, veterinary medicine, ophthalmology, chiropractic care, and more, over time, often with promotional financing.
Further reading: Roundtable: Hearing Aid Selection in Severe, Profound Losses
Discussion
We think the time has come for hearing care professionals and hearing aid manufacturers to re-visit and re-emphasize custom products and deep canal impression-taking skills to better address the long-standing hearing aid stigma.
When a healthcare product/solution is obvious, embarrassing, or not attractive to the individual wearing it, the recipient is unlikely to seek the solution, as it may be (to the recipient) worse than the problem it solves. This may well be the essence of the hearing aid stigma.
Psychotherapists are taught to match the patient’s language and their “third umpire construction of reality” to decrease resistance to interventions. For example, when responding to a patient who emphasizes the pleasure of feeling the sand at a beach resort, the therapist would not predominantly refer to the visual or auditory beauty of the beach. Rather, the therapist would reference kinesthetic cues. The therapist would understand what is most important to the patient (for example, cosmetic issues) and would use that information to meet the patient where she is, to satisfy the patient’s needs and concerns.
However, for people with age-related hearing loss who need to hear and listen more effectively but absolutely do not want to wear visible hearing aids, the most common offering and the thing they don’t want to wear are traditional RIC, RITEs, and BTEs. Sometimes, if we don’t address the hearing aid stigma and we only offer visible products, the patient may perceive that we are more or less saying, “Get over it, it’s good for you.” In that scenario we dismiss or ignore the hearing aid stigma, even though it is probably there (spoken or unspoken). Indeed, even if it’s not spoken, we should suspect it is present.
As hearing healthcare professionals, we need to be cognizant of the personal and very important choices people make. The perceived stigma and cosmetic disadvantages associated with visible hearing aids are real for many people. These perceptions are important and need to be anticipated, acknowledged, and managed. Further, prescription and OTC products with tulip dome fittings are rarely the best acoustic solution for anyone, although they are admittedly sometimes preferred by patients and consumers as they are easy to try to fit, and offer little (if any) occlusion.
For most people with mild-to-moderate hearing loss, tiny, almost invisible, hardly visible, custom-made, deep insertion hearing aids and earmolds (not off-the-shelf generic premium RITE products with domes…) are worthy of re-consideration. For those with more significant thresholds such as 65-90 dB, more powerful RICS and RITES with custom deep-fitting earmolds are often the better choice.
Sure, we can keep telling patients their hearing loss is more visible than their hearing aids. But then, we should also admit that only 10% of people with hearing loss in the USA acquire hearing aids.(3) As Albert Einstein reportedly said, “The definition of insanity is doing the same thing over and over and expecting a different result.”
Visible hearing aids announce a personal problem to the world. For many patients, it’s not an attractive way to handle their medical problem(s). We should respect the patient’s “third umpire constructions” of their reality and we should be more aware of spoken and unspoken hearing aid stigmas to be more patient-centered in our approach to treating hearing and listening problems.
About the Authors: Douglas L. Beck, AuD, F-AAA, CCC-A, is among the most prolific authors in audiology. He is the co-host of The Hearing Matters Podcast. His publications address a wide variety of audiology, clinical, academic, and professional topics. He can be reached at [email protected] or www.douglaslbeck.com. Michael A. Harvey, PhD, is a clinical psychologist who practices in Framingham, Mass. His most recent books are Odyssey of Hearing Loss: Tales of Triumph and Listen with the Heart: Relationships and Hearing Loss, both published by DawnSignPress. Feedback is welcome at [email protected].
References
- Harvey M. Aging with Dignity with Assistance From an Audiologist. Hearing Review. 2023;14-17.
- Kochkin S, Rogin C. Quantifying the obvious: the impact of hearing aids on quality of life. Hearing Review. 2000;7(1):8-34.
- Haile LM, Orji AU, Reavis KM, et al. Hearing Loss Prevalence, Years Lived With Disability, and Hearing Aid Use in the United States From 1990 to 2019: Findings From the Global Burden of Disease Study. Ear Hear. 2024;45(1):257-267. doi:10.1097/AUD.0000000000001420
- Levy B. Breaking the Age Code: How Your Beliefs About Aging Determine How Long and Well You Live. New York, NY: William Morrow; 2022.
- Amlani AM. It’s not immoral to increase hearing aid prices in an inelastic market. Hearing Review 2009;16(1):12–16.
- Wallhagen MI. The stigma of hearing loss. Gerontologist. 2010 Feb;50(1):66-75. doi: 10.1093/geront/gnp107. Epub 2009 Jul 10. PMID: 19592638; PMCID: PMC2904535. Available at: https://academic.oup.com/gerontologist/article/50/1/66/692298
- Alcido M, Forbes. Forbes Health Survey: Nearly Half Of People With Hearing Loss Believe There Is A Hearing Aid Stigma. April 16, 2024. Available at: https://www.forbes.com/health/hearing-aids/hearing-aids-stigma-survey/
- Novak S. For Many, Stigma of Hearing Loss Brings Trouble; Here’s What May Help. February 21, 2024. Available at: https://www.webmd.com/alzheimers/news/20240221/hearing-aids-bring-stigma-for-many
- Beadle J, Jenstad L, Cochrane D, Small J. Perceptions of older and younger adults who wear hearing aids. Int J Audiol. Published online January 23, 2024. doi:10.1080/14992027.2024.2305279
- Nickbakht M, Ekberg K, Waite M, et al. The experience of stigma related to hearing loss and hearing aids: perspectives of adults with hearing loss, their families, and hearing care professionals. Int J Audiol. Published online June 2, 2024. doi:10.1080/14992027.2024.2353862
- National Council on Aging. 5 Best Over-the-Counter (OTC) Hearing Aids of 2024. September 3, 2024. Available at: (https://www.ncoa.org/adviser/hearing-aids/best-otc-hearing-aids/)
- Sieber T. Best Buy Hearing Aids: A Review of OTC Models, Features, Prices, and Lab Test Performance. July 16, 2024. Available at: https://www.hearingtracker.com/hearing-aids/best-buy-otc-hearing-aids
- NASDAQ. Suze Orman Explains Why Most Americans Can’t Afford a $500 Emergency Expense. August 24, 2024. Available at: https://www.nasdaq.com/articles/suze-orman-explains-why-most-americans-cant-afford-a-$500-emergency-expense