Inside the Research | September 2022 Hearing Review
Although there is still no cure for chronic tinnitus, there are methods to help sufferers improve their situation and quality of life.
By Dr Maren Stropahl
Even though there is no cure for tinnitus today, good approaches that significantly reduce the burden of affected individuals are available. Therefore, it is hoped that the message to sufferers that they have to “live with their tinnitus” will become less and less pronounced.
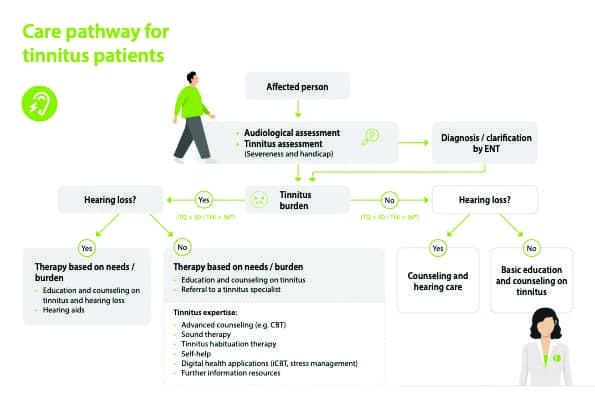
The word tinnitus comes from the Latin word “tinnire,” which means “to ring,” and describes the perception of a sound without being able to attribute it to an external sound source. This type of tinnitus is therefore a purely subjective sensation and can only be perceived by the person affected.1 It is estimated that about 10-15% of the population experience tinnitus.1,2 However, not all tinnitus is the same. The majority of people who experience tinnitus do not find it disturbing, but about 20% of people with tinnitus need clinical support to cope with the noise.3 About 2% of those affected suffer so severely that their daily lives and quality of life are significantly impaired2 (see Chart 1). The coronavirus pandemic could exacerbate this effect.
Facts About Tinnitus. Top left: Prevalence; top right: Potential triggers of tinnitus; Bottom left: Distribution of impairment; Bottom right: prevalence of hearing loss among people with tinnitus. Copyright by Sonova Audiological Care
The exact cause of tinnitus has not been definitively determined to date. Experts nowadays believe that tinnitus is not just a problem of the auditory organ, but originates either in the peripheral, central, or even outside auditory brain regions. It is most likely a complex interaction between central and peripheral mechanisms and is usually associated with some form of hearing loss.1,2 It has been shown that in the case of tinnitus there is often abnormal overactivity of neurons in the brain, as well as abnormal synchronous firing activity of neurons.2,6 It seems that not only the auditory centers of the brain affected because other cortical networks also show an alteration. Recent findings lead to the assumption that a large proportion (about 90%) of people with tinnitus have a hearing loss, even if it is not always measurable.1 In addition to hearing loss, the development of tinnitus is often associated with age, increased noise exposure, and stress.1,7
Tinnitus is considered acute if its onset is perceived within the last 3 months and chronic when it persists for more than 6 months.1 The approaches to treatment for acute and chronic tinnitus are very different and for the purpose of this summary, only chronic tinnitus will be considered. The perception of the sound can be either constant or intermittent, it is often perceived either in one or both ears or inside the head. Some sufferers find it difficult to localize the sound specifically. Tinnitus can be either tonal, in which case the frequency of the sound can be precisely determined by special methods, or atonal (noisy), which corresponds more to a sound composed of several frequencies.
Tinnitus is not referred to as an actual disease, but as a symptom and a change in how someone perceives their own hearing. As a consequence of suffering from tinnitus, however, a serious medical condition can develop. The suffering of the affected person is usually not caused by hearing the sound, but by the negative, emotional reaction caused by the perceived sound. So far, there are no clinically applicable objective measures to diagnose tinnitus,8 but standardized subjective tools exist in different languages to determine the severity of tinnitus.
Often, the most important concern for people experiencing tinnitus is to find out where the perceived noise is coming from and whether it is related to a more severe condition. A survey has shown that more than 90% of sufferers get their first information from the Internet.9 Compared to hearing-impaired people, people with tinnitus seek professional support very early after the onset of the symptom. An analysis showed that 71% of those affected contacted a professional within the first year after the onset of tinnitus, 45% even within the first three months. Unfortunately, many sufferers who seek specialist help often experience a misguided path and rarely receive direct support.10
Most individuals who suffer from tinnitus desire a pharmacological solution that will make the tinnitus disappear or at least become quieter.11,12 To date, there is no cure for tinnitus, however recent studies and guidelines show that there are some successful approaches to significantly reduce the tinnitus burden and significantly improve the quality of life.12 Through a multidisciplinary approach and individually tailored therapy, a large proportion of sufferers can learn to cope with the symptom and lead a life without major impairment.(1, 3, 12, 13)
In recent years, clinical guidelines have been developed and published by international tinnitus experts to assist various medical professions in recognizing affected individuals and suggesting individualized measures for improvement (eg, European Tinnitus Guidelines, NICE guidelines [UK], Clinical Practice Guidelines).(1,15,3) The experts agree that the treatment of tinnitus requires an anamnesis and diagnosis in order to characterize the condition individually and, if necessary, to exclude medical causes. The so-called tinnitus assessment is used to identify how the tinnitus affects the individual’s daily life, ie, whether there are problems falling asleep, the tinnitus occurs primarily in certain situations, or whether the tinnitus interferes with certain activities of daily living. Another prerequisite for the next steps of management is the adequate education of the affected person. It is important that a person suffering from tinnitus understands what the possible causes of tinnitus are, what the connections are, eg, to hearing loss, and which treatment methods are available.1 This education can take place through a counseling session or, for example, through digital offerings. It is also important to inform about myths and misinformation that are circulating and to provide them with trustworthy sources for obtaining information.
The range of treatments for tinnitus is diverse, but not all approaches are recommended. Many methods lack systematic investigation and review of the evidence of clinical benefit. Current guidelines provide recommendations on existing treatment methods. For example, currently, the European guideline recommends cognitive behavioral therapy (CBT) as the best-validated therapy for tinnitus.1 Accordingly, CBT is currently the gold standard of tinnitus treatment and shows success in improving the tinnitus burden for many sufferers. (16-21) The goal of CBT is to change maladaptive behaviors and negative associations that arise from the perception of tinnitus. This change causes sufferers to neutralize their negative perceptions towards tinnitus and thus the symptoms have less of an impact on their lives. Access to CBT with professional guidance is often associated with long waiting times and high costs. Recent efforts to provide this type of therapy online and self-directed are showing initial success. Internet-based CBT shows similarly good results as conventional CBT in the studies. (19-22)
Noise therapy is one of the oldest and best-known interventions for tinnitus.1 The term noise therapy covers very different methods, which usually have the goal that the tinnitus is “masked” and thus the attention can be diverted away from the disturbing noise. Accordingly, classical noise therapy does not treat the cause of tinnitus but serves as an acute solution for the affected person to reduce the negative consequences of the tinnitus perception in certain situations. For this purpose, sounds such as pleasant music or a neutral, constant noise are often used.23,24 Although this approach is widely used, there are few high-quality studies that sufficiently demonstrate the clinical benefit. In particular, it is not possible to say unequivocally which type of noise therapy provides the greatest benefit.1
One type of noise therapy is the hearing aid. Hearing aids can mask the tinnitus by amplifying the surrounding sounds, thus directing attention away from the tinnitus.(25-29) Hearing aids are only recommended for tinnitus treatment when hearing loss is present.1 Since approximately 80-90% of tinnitus patients have some type of hearing loss, it is recommended that an audiological examination be performed and that both an audiogram and speech understanding be measured.1,30 Most modern hearing aids have an integrated tinnitus function to play additional neutral sounds in the background. The standard offering includes noise generators using white and or pink noise. More recent noise generators also provide modulated noise or the possibility to play back preferred noises. The evidence for the efficacy of these noise generators is not clear, however, this method has low risks when used correctly. Hearing aids with integrated tinnitus functions are therefore a good method to improve the hearing function and additionally to have an option to influence the tinnitus in everyday life.(1,29,31)
Newer approaches to noise therapy go a step further and more specifically target the cause of tinnitus. These include, for example, acoustic neuromodulation, which aims to alter unusual neuronal activity and cortical reorganization associated with tinnitus. An example is “notched-music” or “notched-noise” therapy, in which music or noise is filtered in such a way that the predetermined tinnitus frequency is eliminated.32 This method can only be applied for tonal tinnitus where the frequency can be determined. There have been studies that have evaluated this approach, however, the results have been inconclusive. Although it may bring improvement to some sufferers, this therapeutic approach is not currently recommended by international guidelines.1,14 Another example is Acoustic coordinated reset neuromodulation.33 This therapy aims to reset the abnormal synchronous firing activity of neurons. According to the studies, sufferers with this method perceive a benefit up to 12 months after the end of therapy. A recent study was able to show that this form of neuromodulation achieves similarly good results as CBT for tinnitus.34 However, based on the data available to date, this method is not currently recommended by the guidelines.1,14 Other neuromodulation methods, such as transcranial electrical stimulation or bimodal stimulation, are currently being evaluated in studies, but the data are not yet sufficient for a reliable statement.1,35
In order to provide people suffering from tinnitus with the best possible treatment, the current consensus among tinnitus experts is that treatment should be individually tailored and embedded in a multidisciplinary network of different specialists.(1,13,36) In the field of audiology, hearing care professionals (HCPs) play an important role. The first point of contact for those affected is usually the general physician or the ENT doctor. After a diagnosis has been made and medical reasons for the tinnitus have been ruled out, further steps can be planned. Since tinnitus is often accompanied by hearing loss, HCPs are the most logical next stop on the patient journey. In addition, HCPs usually spend more time with the individual suffering from tinnitus and can integrate the hearing care into tinnitus counseling. It is important to understand how tinnitus and hearing loss are related and why hearing aids can help tinnitus with concomitant hearing loss.26,37 Depending on the severity of the tinnitus, further treatment steps may be necessary for those affected. HCPs with additional training can provide more in-depth counseling eg, based on Tinnitus Retraining Therapy (TRT).38 Nowadays, there are also digital or Internet-based solutions for sufferers that can be recommended by HCPs and physicians. For the more severely affected individuals, a referral to an appropriate professional (eg, ENT doctors, psychologists, or other tinnitus experts) should be recommended.
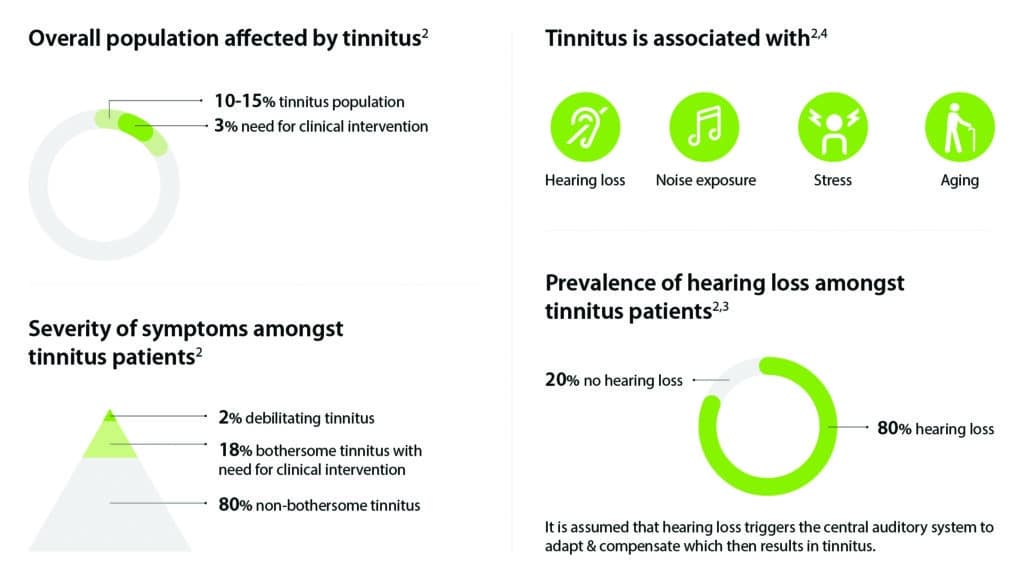
Many HCPs do not have sufficient additional training in tinnitus management, which represents a gap in the current care pathway. Educational institutions and hearing aid manufacturers are currently trying to close this gap by offering courses. Tinnitus experts from clinical practice also show simple methods and standardized ways how HCPs can proceed in case of tinnitus complaints to ensure the best possible treatment for affected persons (see Chart 2). It is important that HCPs build their interdisciplinary network to treat those with more significant levels of tinnitus severity in collaboration with other experts.
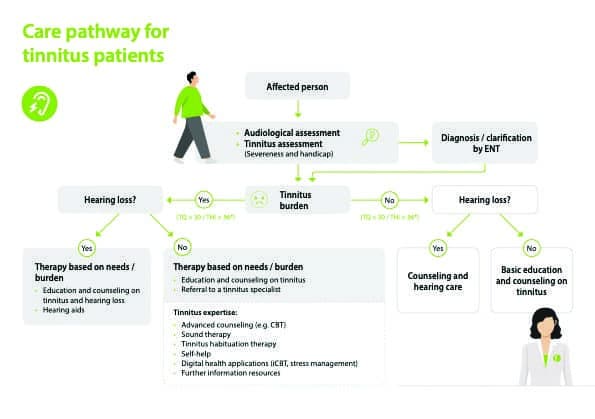
Chart 2: Schematic representation of the care pathway for tinnitus. Reproduced based on (1,30)
A look into the future indicates that the tinnitus problem could become bigger rather than smaller due to today’s noise pollution and additional environmental influences. Even though there is no cure for tinnitus today, good approaches that significantly reduce the burden of affected individuals are available. Therefore, it is hoped that the message to sufferers that they have to “live with their tinnitus” will become less and less pronounced. Professionals should motivate the affected persons and identify which methods are available to significantly improve their quality of life and to remove the “symptom tinnitus” from the center of their lives.
Citation for this article: Stropahl M. Why the one-size-fits-all approach to tinnitus is not successful. Hearing Review. 2022;29(9):28-31.
References
- Cima RFF, Mazurek B, Haider H, et al. A multidisciplinary European guideline for tinnitus: Diagnostics, assessment, and treatment. HNO. 2019;67(S1):S10-S42.
- Baguley D, McFerran D, Hall D. Tinnitus. The Lancet. 2013;382(9904):1600-1607.
- Tunkel DE, Bauer CA, Sun GH. Clinical Practice Guideline: Tinnitus. Otolaryngology-Head and Neck Surgery. 2014;151(S2):S1-S40.
- Beukes E, Manchaiah V. The impact of the COVID-19 pandemic on tinnitus. The Hearing Journal. 2021;74(4):10-11.
- Schlee W, Holleland S, Bulla J, et al. The effect of environmental stressors on tinnitus: A prospective longitudinal study on the impact of the COVID-19 pandemic. Journal of Clinical Medicine. 2020;9(9):2756.
- Haider HF, Bojic T, Ribeiro SF, Paco J, Hall DA, Szczepek AJ. Pathophysiology of subjective tinnitus: Triggers and maintenance. Frontiers in Neuroscience. 2018;12(866):1-16.
- Shore SE, Roberts LE, Langguth B. Maladaptive plasticity in tinnitus-Triggers, mechanisms and treatment. Nature Reviews Neurology. 2016;12:150-160.
- Jackson R, Vijendren A, Phillips J. Objective measures of tinnitus: A systematic review. Otology & Neurotology. 2019;40(2):154-163.
- Tyler R, Perreau A. Managing patient—and audiologist—expectations for tinnitus treatment. The Hearing Journal. 2019;72(3):16-19.
- McFerran D, Hoare DJ, Carr S, Ray J, Stockdale D. Tinnitus services in the United Kingdom: A survey of patient experiences. BMC Health Services Research. 2018;18(110):1-13.
- Husain FT, Gander PE, Jansen JN, Shen S. Expectations for tinnitus treatment and outcomes: A survey study of audiologists and patients. Journal of the American Academy of Audiology. 2018;29(04):313-336.
- McFerran DJ, Stockdale D, Holme R, Large CH, Baguley DM. Why is there no cure for tinnitus? Frontiers in Neuroscience. 2019; 13(802):1-13.
- Henry J, McMillan L, Manning C. Multidisciplinary tinnitus care. The Journal for Nurse Practitioners. 2019;15(9):671-675.
- The American Speech-Language-Hearing Association (ASHA) website. German S3 guideline 017/064: Chronic Tinnitus. Germany: Association of the Scientific Medical Societies, (AWMF-Register Nr. 017/064 Klasse: S3 Chronischer Tinnitus). https://apps.asha.org/EvidenceMaps/Articles/ArticleSummary/41d25297-dbce-42ab-80c2-971891e0c2be. Published May 2018.
- National Institute for Health and Care Excellence (NICE) website. NICE Guideline [NG155]. Tinnitus: Assessment and Management. https://www.nice.org.uk/guidance/ng155. Published March 11, 2020.
- Cima RFF, Andersson G, Schmidt CJ, Henry JA. Cognitive-behavioral treatments for tinnitus: A review of the literature. J Am Acad Audiol. 2014;25(1):29-61.
- Cima RFF, Maes IH, Joore MA, et al. Specialised treatment based on cognitive behaviour therapy versus usual care for tinnitus: A randomised controlled trial. The Lancet. 2012;379(9830):1951-1959.
- Landry EC, Sandoval XCR, Simeone CN, Tidball G, Lea J, Westerberg BD. Systematic review and network meta-analysis of cognitive and/or behavioral therapies (CBT) for tinnitus. Otology & Neurotology. 2020;41(2):153-166.
- Weise C, Kleinstäuber M, Andersson G. Internet-delivered cognitive-behavior therapy for tinnitus: A randomized controlled trial. Psychosomatic Medicine. 2016;78(4):501-510.
- Beukes EW, Manchaiah V, Allen PM, Baguley DM, Andersson G. Internet-based cognitive behavioural therapy for adults with tinnitus in the UK: Study protocol for a randomised controlled trial. BMJ Open. 2015;5:e008241.
- Jasper K, Weise C, Conrad I, Andersson G, Hiller W, Kleinstauber M. Internet-based guided self-help versus group cognitive behavioral therapy for chronic tinnitus: A randomized controlled trial. Psychotherapy and Psychosomatics. 2014;83(4):234-246.
- Heinrich S, Rozental A, Carlbring P, Andersson G, Cotter K, Weise C. Treating tinnitus distress via the Internet: A mixed methods approach of what makes patients seek help and stay motivated during Internet-based cognitive behavior therapy. Internet Interventions. 2016;4(2):120-130.
- Searchfield GD, Durai M, Linford T. A state-of-the-art review: Personalization of tinnitus sound therapy. Frontiers in Psychology. 2017;8(1599):1-11.
- Henry JA, Quinn CM. Sound therapy for tinnitus: Options for audiologists. Perspectives. 2020;5(3):669-683.
- Yokota Y, Yamashita A, Koyama S, Kitano K, Otsuka S, Kitahara T. Retrospective evaluation of secondary effects of hearing aids for tinnitus therapy in patients with hearing loss. Auris Nasus Larynx. 2020;47(5):P763-P768.
- Searchfield GD. Hearing aids for tinnitus. In: Baguely DM, Fagelson M, eds. Tinnitus: Clinical and Research Perspectives. Plural Publishing; 2015.
- Hoare DJ, Edmondson-Jones M, Sereda M, Akeroyd MA, Hall D. Amplification with hearing aids for patients with tinnitus and co-existing hearing loss. Cochrane Database of Systematic Reviews. 2014;1CD010151.
- Tutaj L, Hoare DJ, Sereda M. Combined amplification and sound generation for tinnitus: A scoping review. Ear and Hearing. 2018;39(3):412-422.
- Sereda M, Xia J, El Refaie A, Hall DA, Hoare DJ. Sound therapy (using amplification devices and/or sound generators) for tinnitus. Cochrane Database of Systematic Reviews. 2018;(12):CD013094.
- Henry JA, Manning C. Clinical protocol to promote standardization of basic tinnitus services by audiologists. American Journal of Audiology. 2019;28(1S):152-161.
- Tutaj L, Hoare DJ, Sereda M. Combined amplification and sound generation for tinnitus: A scoping review. Ear and Hearing. 2018;39(3)412-422.
- Pantev C, Rudack C, Stein A, et al. Study protocol: Münster tinnitus randomized controlled clinical trial-2013 based on tailor-made notched music training (TMNMT). BMC Neurology. 2014;14(40):1-8.
- Tass PA, Adamchic I, Freund H-J, Von Stackelberg T, Hauptmann C. Counteracting tinnitus by acoustic coordinated reset neuromodulation. Restorative Neurology and Neuroscience.2012;30(2):137-159.
- Theodoroff SM, McMillan GP, Schmidt CJ, et al. Randomised controlled trial of interventions for bothersome tinnitus: Desyncra versus cognitive behavioural therapy. International Journal of Audiology. 2021.DOI: 10.1080/14992027.2021.2004325.
- Langguth B. Non-invasive neuromodulation for tinnitus. Journal of Audiology & Otology. 2020;24(3):113-118.
- Baguley, D, Andersson G, McFerran D, McKenna L, eds. Tinnitus: A Multidisciplinary Approach. 2nd ed. Wiley; 2013.
- Searchfield GD, Kaur M, Martin WH. Hearing aids as an adjunct to counseling: Tinnitus patients who choose amplification do better than those that don’t. International Journal of Audiology. 2010;49(8):574-579.
- Jastreboff PJ, Tyler RS. Tinnitus habituation therapy (THT) and tinnitus retraining therapy (TRT). In: Tyler RS, ed. Tinnitus Handbook. Singular Publishing; 2000:357-376.